Substance use in the United States is not evenly distributed across age groups.
The strongest national datasets, including SAMHSA National Survey on Drug Use and Health NSDUH 2023, CDC overdose mortality surveillance through 2024, and Monitoring the Future youth surveys, show a consistent pattern: experimentation and binge behaviors peak in late adolescence and young adulthood, chronic dependence and medical complications concentrate in midlife, and prescription drug interactions plus alcohol risks increase again among older adults.
Alcohol remains the most widely used substance across adulthood, nicotine vaping dominates youth nicotine exposure, cannabis is the most common illicit drug across nearly all ages, and opioid related deaths are highest in people roughly 30 to 50, even though use prevalence is not highest in that group.
Table of Contents
ToggleOverall Substance Use Disorder Prevalence by Age
The clearest snapshot comes from NSDUH 2023, which measures both use and diagnosable substance use disorder. Young adults aged 18 to 25 consistently show the highest rates of substance use disorder, followed by adults over 26, while adolescents show lower but still significant rates.
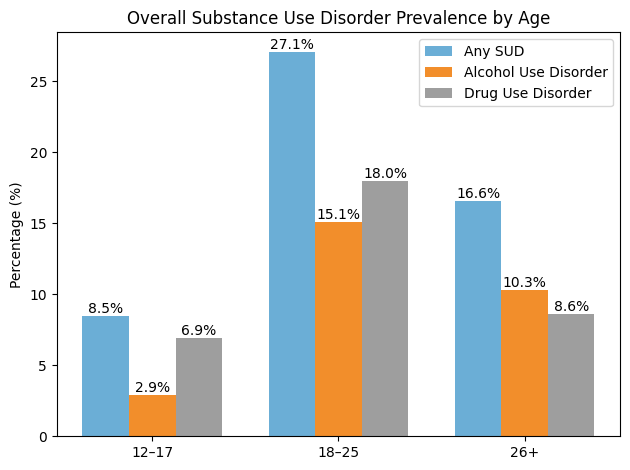
These figures confirm that young adulthood remains the highest vulnerability period overall. Transition stress, social exposure, college environments, employment instability, and mental health pressures all contribute.
However, adults over 26 still represent a large absolute number of cases because the population size is larger and substance use tends to persist longer.
Alcohol: The Most Common Substance Across Adulthood
Alcohol remains the dominant psychoactive substance in the United States, but how it is used changes significantly by age. Monthly alcohol use is slightly higher among adults over 26 compared with young adults, yet binge drinking peaks in the younger group.
Past Month Alcohol Indicators NSDUH 2023
12 to 17
18 to 25
26 plus
Alcohol use
6.9 percent
49.6 percent
51.9 percent
Binge drinking
3.9 percent
28.7 percent
22.7 percent
Heavy alcohol use
0.5 percent
6.9 percent
6.2 percent
Alcohol trends in the US show that people drink less frequently overall than older adults but consume larger amounts per occasion. That pattern explains why alcohol related injuries, assaults, and acute intoxication hospital visits are heavily concentrated among people in their late teens and twenties.
Among older adults, alcohol risks shift toward chronic disease interactions. Hypertension, liver disease, medication conflicts, and sleep disorders become the main clinical concerns rather than binge intoxication.
Cannabis: Widespread Across Ages, but Used Differently
Cannabis has become the most commonly used illicit substance nationally. Legalization in many states has increased access, but usage style varies strongly with age.
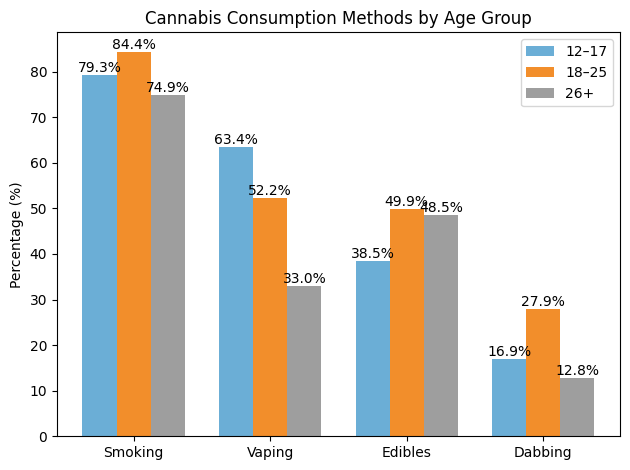
Data shows the highest reliance on vaping devices, largely due to concealability, perceived safety, and device culture. Young adults use the broadest mix, including high-potency concentrates. Older adults show more edible consumption, often tied to medical cannabis use for pain or sleep.
Higher potency products complicate risk assessment because THC concentrations today are significantly higher than a decade ago, increasing dependence potential and psychiatric side effects.
Nicotine: Major Generational Shift Toward Vaping
Nicotine use illustrates one of the clearest generational divides. Traditional cigarette smoking has declined substantially among adolescents but has been replaced by electronic nicotine delivery systems.
Among Past Month Nicotine Users NSDUH 2023
12 to 17
18 to 25
26 plus
Exclusive nicotine vaping
74.9 percent
47.6 percent
15.7 percent
Tobacco only, no vaping
8.6 percent
19.6 percent
68.2 percent
Mixed-use vaping plus tobacco
Moderate
Moderate
Lower
Teen nicotine exposure is therefore primarily vape-driven. Adults over 26 still rely mostly on combustible tobacco, which carries a higher long-term disease risk but often lower nicotine delivery intensity compared with some modern vaping products.
Nicotine vaping is common among adolescents. This JAMA Insights article reviews the health effects of vaping among youth in the US and current recommendations for screening and treatment. https://t.co/KTaL5U4OeX pic.twitter.com/0vpG7W9kG0
— JAMA (@JAMA_current) September 7, 2024
Monitoring the Future 2024 data confirms declining youth vaping overall, yet daily nicotine vaping among high school seniors remains in the mid single-digit percentage range, enough to sustain addiction pipelines.
Stimulants and Opioids: Prevalence versus Harm
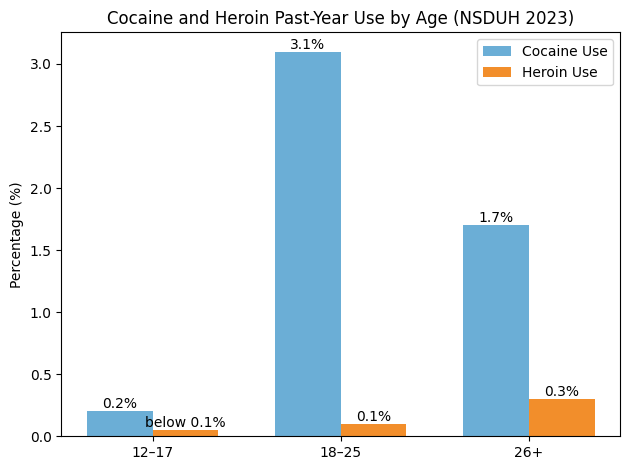
Illicit stimulant use, such as cocaine, e shothe ws highest prevalence among young adults, while opioid related harm, including overdose deaths, peaks later.
Cocaine and Heroin Past-Year Use NSDUH 2023
Overdose Mortality: Highest in Midlife
CDC provisional data released early 2026 show overdose death rates declining overall from 2023 to 202,4 but still heavily concentrated amonmiddle-ageded adults.
Drug Overdose Death Rate Per 100000
2023
2024
Ages 15 to 24
13.5
8.5
Ages 35 to 44
60.8
44.2
Ages 65 plus
14.7
13.4
Even with improvement, adults aged roughly 35 to 44 experience overdose mortality rates several times higher than youth. This reflects cumulative addiction history, chronic health conditions, stronger opioids, and polysubstance mixing, including alcohol, benzodiazepines, and stimulants.
Adolescents: Experimentation but Declining Overall Prevalence
View this post on Instagram
A post shared by Longevity-NOW-FL | Prof Luigi Fontana, MD, PhD, FRACP (@fontana2311)
Youth surveys show declining alcohol and cigarette use compared with previous decades. However, risks have shifted rather than disappeared. Key characteristics include:
Because adolescent brains continue developing into the mid twenties, exposure during this period increaseslong-termm addiction vulnerability.
Young Adults: Peak Intensity Phase
Ages 18 to 25 represent the highest combined risk period across substances. Several drivers explain this concentration:
This group leads in binge drinking, cannabis concentrate use, stimulant experimentation, and polysubstance mixing. Preventive strategies in this age range often focus on screening, brief interventions, and mental health integration.
Middle Adulthood: Chronic Dependence and The Highest Mortality

From roughly age 30 onward, patterns shift from experimentation toward sustained dependence. Prescription opioid exposure, chronic pain, job stress, and financial pressure contribute. Harm escalates even if prevalence does not increase.
Polysubstance use becomes particularly dangerous in this phase:
This explains why overdose mortality peaks despite lower experimentation rates.
@thebeautyofdata Cause of deaths by substance abuse in the USA #opioidepidemic #alcohol #thebeautyofdata ♬ Coffin Dance – Music Falcon
Older Adults: Prescription Interaction Risks
Among adults over 55, substance misuse increasingly involves:
Age-related metabolic changes reduce drug clearance, increasing overdose risk even at lower doses. Social isolation and chronic illness also influence substance use.
Key Takeaways Across the Lifespan
Substance use evolves predictably with age:
Life Stage
Dominant Risk Substances
Primary Drivers
Adolescents
Nicotine vaping and cannabis experimentation
Peer influence, curiosity, and digital culture
Young adults
Alcohol, binge, cannabis concentrates, stimulants
Social transition stress independence
Middle age
Alcohol, opioid, and polysubstance use
Chronic stress, health issues, and dependence
Older adults
Prescription interactions with alcohol and cannabis
Pain management, sleep problems, and isolation
Prevalence alone does not predict harm. Younger groups show higher experimentation, while middle-aged adults show higher mortality and chronic health impact.
Bottom Line

Substance abuse in the United States follows a life course pattern rather than a uniform epidemic. Adolescents encounter nicotine and cannabis primarily through modern delivery systems.
Young adults drive binge drinking and high-intensity recreational drug use. Middle-aged adults carry the highest overdose mortality burden, largely due to opioids and polysubstance exposure.
Older adults face increasing risks from medication interactions and alcohol related disease. Effective prevention, therefore, requires age-specific strategies rather than a single national approach.