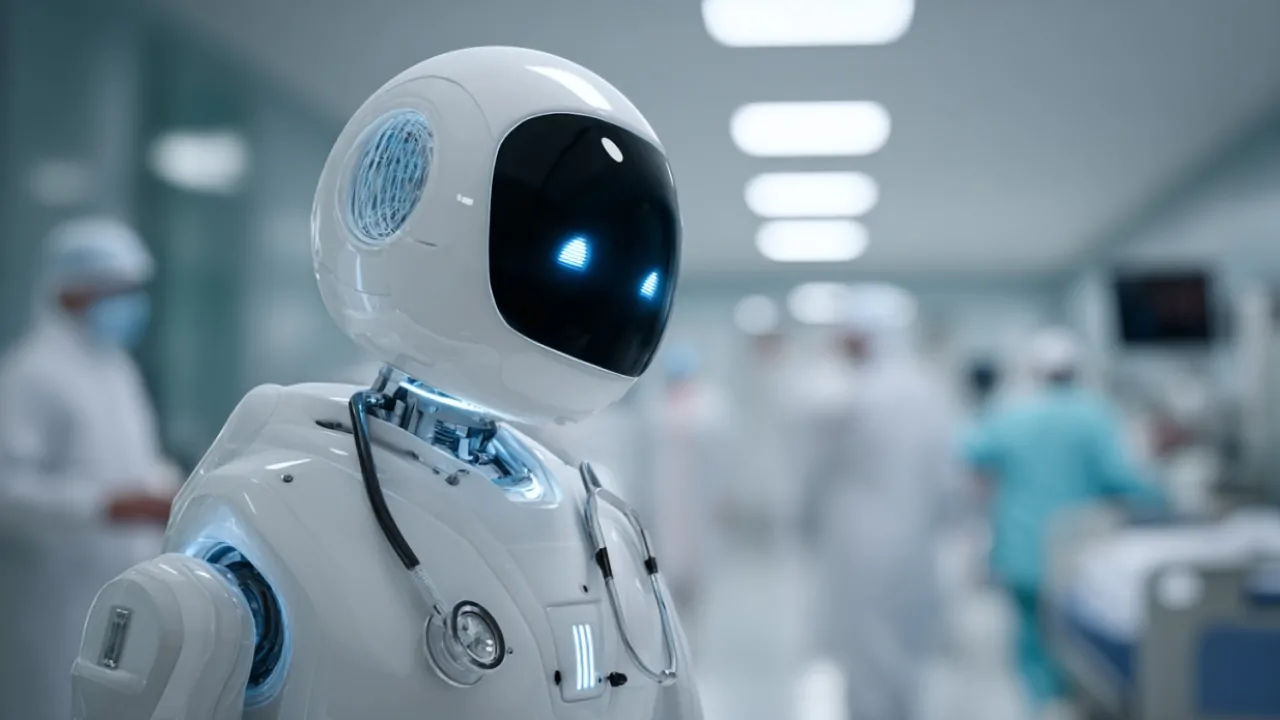
Artificial intelligence already plays a significant role inside hospitals, mainly in diagnostics, imaging analysis, administrative work, and decision support.
However, full replacement of doctors is not close.
Current evidence shows AI improves efficiency and diagnostic accuracy when combined with human clinicians, but it still lacks clinical judgment, accountability, and interpersonal skills required in real patient care.
The realistic outcome for the foreseeable future is collaboration rather than replacement.
Where AI Is Already Used In Hospitals
AI deployment in healthcare has accelerated over the past decade, especially in areas that rely heavily on data analysis. Hospitals increasingly integrate machine learning tools into daily workflows, but these systems typically support clinicians rather than operate independently.
Radiology and pathology are the most advanced adoption areas because medical imaging produces structured data that AI can analyze efficiently. Algorithms now assist in detecting tumors, fractures, stroke indicators, retinal disease, and lung abnormalities.
Studies show AI systems can match or sometimes exceed average physician accuracy in specific imaging tasks, especially when trained on large datasets.
Administrative work has also shifted toward automation. Hospitals face heavy documentation requirements, and AI tools now transcribe consultations, generate medical notes, handle billing codes, and assist with appointment triage.
This reduces physician workload rather than eliminating physicians.
Predictive analytics represents another expanding area. AI models analyze electronic health records to identify patients at risk for complications such as sepsis, heart failure, or hospital readmission.
These tools help clinicians intervene earlier but do not replace clinical decision-making.
Current AI Applications In Hospitals
Area
Typical AI Role
Impact On Doctors
Medical imaging
Scan interpretation support
Faster diagnosis
Documentation
Automated note generation
Less paperwork
Risk prediction
Disease risk alerts
Earlier intervention
Clinical decision support
Treatment suggestions
More informed decisions
Scheduling and admin
Workflow automation
Efficiency improvement
These applications demonstrate augmentation rather than substitution.
Diagnostic Accuracy: AI Versus Doctors

Diagnostic performance comparisons often attract attention because diagnosis seems like a core physician task. AI performs strongly in narrow diagnostic contexts, especially image recognition or structured data analysis.
However, clinical diagnosis involves more than pattern recognition. Doctors interpret symptoms alongside medical history, lifestyle factors, social context, and patient communication. AI struggles when the data are incomplete, inconsistent, or ambiguous.
Research consistently shows that the highest diagnostic accuracy occurs when AI supports clinicians rather than replaces them.
Human oversight remains essential because AI models can misinterpret data, produce confident but incorrect outputs, or miss rare conditions outside training datasets.
Comparative Diagnostic Strengths
Capability
AI Systems
Human Doctors
Pattern recognition
Very strong
Strong
Context understanding
Limited
Strong
Handling rare cases
Weak
Stronger
Patient interaction
Minimal
Essential
Ethical judgment
None
Critical
This balance explains why replacement is not imminent.
Why Full Replacement Is Difficult

Medicine involves uncertainty, ethical responsibility, and complex interpersonal interactions. These aspects limit AI independence.
Clinical judgment requires synthesis of incomplete information. Doctors often make decisions with imperfect data, evolving symptoms, or conflicting evidence. AI typically performs best when conditions are well defined, and data are structured.
Communication also plays a central role. Patients expect explanations, reassurance, and empathy.
Treatment adherence often depends on trust between patient and physician. AI conversational ability continues to improve, but still lacks genuine human rapport.
Legal responsibility presents another barrier. Healthcare operates under strict regulatory frameworks.
If an AI system makes a harmful decision, liability questions arise regarding hospitals, developers, or supervising physicians. Until accountability is clearly defined, an independent AI clinical authority remains unlikely.
Economic And Workforce Drivers Behind AI Adoption
Healthcare systems face rising costs, staff shortages, and increasing data complexity. These pressures accelerate AI integration.
Global projections suggest a substantial shortage of healthcare workers within the next decade. Aging populations increase demand while training new physicians requires years. AI helps bridge capacity gaps without eliminating clinicians.
Cost control is another factor. Administrative inefficiencies consume significant healthcare budgets. AI automation reduces documentation time, optimizes scheduling, and improves resource allocation.
Healthcare data growth also favors AI. Modern hospitals generate large volumes of imaging data, genomic information, wearable sensor data, and electronic records. AI excels at identifying patterns within large datasets that humans cannot easily process.
Key Drivers Of Medical AI Growth
Driver
Explanation
Effect
Workforce shortages
Aging population and limited doctors
AI assistance demand
Rising healthcare costs
Pressure on hospital budgets
Automation adoption
Data expansion
More clinical data generated
AI analysis necessity
Technological advances
Better algorithms and computing power
Increased capability
These forces push adoption but not full automation.
Areas Least Likely To Be Fully Automated
Some medical specialties depend heavily on human interaction, manual skill, or rapid decision-making under uncertain conditions.
These roles remain difficult to automate.
Emergency medicine involves unpredictable situations where doctors adapt quickly without complete data. Surgery requires dexterity, judgment, and adaptability beyond current robotic autonomy.
Psychiatry depends heavily on human communication and emotional understanding. Primary care involves longitudinal relationships that AI cannot replicate effectively.
These fields will likely integrate AI tools without replacing physicians.
Preventive Medicine And Long Term Health Monitoring
One area where AI is expanding quickly is preventive healthcare and longitudinal health tracking. Advanced analytics now combine biometrics, genetic information, imaging data, and lifestyle patterns to assess disease risk earlier than traditional methods.
For example, some personalized health platforms integrate AI-driven diagnostics with comprehensive biological monitoring. Services like Biograph’s longevity health assessment reflect this shift toward proactive medicine, where AI helps identify early aging markers, metabolic risks, and preventive interventions before symptoms appear.
This trend complements clinical medicine rather than replacing hospital physicians, but it demonstrates how AI may reshape patient care pathways outside acute hospital settings.
Preventive AI tools reduce hospital admissions when used effectively, but they still require physician interpretation and medical oversight.
Realistic Timeline Expectations

Predictions vary, but most medical technology experts converge on a gradual transformation rather than a sudden replacement.
In the near term, AI will expand as a clinical assistant. Diagnostic tools, administrative automation, and predictive analytics will become routine in hospitals.
Over the next two decades, semi-autonomous systems may handle specific diagnostic pathways or procedural tasks under supervision. AI may conduct initial patient triage or monitor chronic conditions remotely.
Complete doctor replacement remains speculative and unlikely in mainstream hospital settings due to ethical, legal, and interpersonal constraints.
Expected Progress Timeline
Time Frame
Likely Developments
0–5 years
Routine AI assistance and documentation automation
5–20 years
Advanced diagnostic support, semi-autonomous systems
20+ years
Possible specialized automated clinics, still supervised
The trajectory favors augmentation.
The Most Likely Future: Hybrid Medicine
Healthcare increasingly moves toward a hybrid model combining AI efficiency with human expertise. In this model, AI analyzes data, identifies patterns, and proposes options while physicians interpret results, make final decisions, and communicate with patients.
This approach improves diagnostic accuracy, reduces burnout from administrative tasks, and allows doctors to focus on clinical reasoning and patient interaction.
Hospitals adopting this model often report improved efficiency without compromising patient safety.
Final Perspective
@yourheartdoc AI will help doctors long before replacing us. #ai #medicine #healthcare ♬ original sound – Yourheartdoc
AI is transforming hospital medicine but not replacing doctors. Its strongest impact lies in data processing, diagnostics support, workflow automation, and predictive analytics.
Medicine requires judgment, accountability, ethical reasoning, and human interaction that AI does not yet replicate. The foreseeable future involves collaboration between clinicians and intelligent systems rather than fully automated healthcare.