Cardioversion, a powerful shock that can reset a chaotic heartbeat, can be life-saving, but it’s not without risks. In 2025, about 1 in 1,000 patients won’t make it, a sobering reminder of the stakes involved.
For the 3.5 million Americans living with atrial fibrillation, though, it’s often a risk worth taking, according to Health Central. When performed correctly, the procedure has a success rate of over 90%, helping many regain a steady rhythm.
But the picture changes in emergencies. When cardioversion happens outside a hospital, the risk of death jumps to 0.4%, underscoring just how much timing and setting matter.
Table of Contents
ToggleKey Takeaways
1. Risk Increase in Repeat Cardioversion: Mortality Rises to 0.15%
For patients who undergo multiple cardioversion procedures, the mortality rate increases to approximately 0.15%, as noted by NCBI.
The elevated risk in these cases may be due to the cumulative stress on the heart from multiple electrical shocks, as well as the progression of underlying heart disease.
Patients requiring repeat cardioversion often have more complex medical histories, which can contribute to higher complication rates.
Additionally, frequent recurrences of arrhythmia may indicate a more refractory form of the disease, necessitating a reassessment of the overall treatment strategy.
Alternative approaches, such as catheter ablation or the implementation of antiarrhythmic drug therapy, may be considered to reduce the need for repeated cardioversion and to manage the arrhythmia more effectively, as noted by Johns Hopkins Medicine.
A comprehensive evaluation of the patient’s condition, including assessing potential triggers and optimizing concomitant medical therapies, is essential to improve long-term outcomes and minimize risks associated with repeated procedures.
2. Elective Cardioversion Under Anesthesia: Lowest Death Rate at 0.02%
Elective cardioversion performed under anesthesia in a controlled environment has a notably low mortality rate of approximately 0.02% according to Research Gate.
The use of anesthesia enhances patient comfort and minimizes movement during the procedure, facilitating the successful delivery of the electrical shock and reducing the likelihood of complications.
The controlled setting allows for comprehensive pre-procedure assessments, including the evaluation of anticoagulation status and the exclusion of left atrial thrombi, which are critical steps in mitigating the risk of thromboembolic events.
Continuous monitoring during and after the procedure ensures that any adverse reactions are promptly identified and managed according to NIH.
The low mortality rate in this context reflects the benefits of meticulous planning, patient selection, and adherence to established protocols.
It also underscores the importance of performing elective cardioversion in settings equipped with the necessary resources and personnel to handle potential emergencies, thereby enhancing patient safety and procedural success.
3. 1 in 1,000 Patients Face Fatal Complications
Cardioversion is a medical intervention designed to restore normal heart rhythm in patients experiencing arrhythmias such as atrial fibrillation (AF) or atrial flutter.
While the procedure is generally considered safe and effective, it is not devoid of risks. The overall mortality rate associated with cardioversion is approximately 0.1%, equating to 1 in 1,000 patients, as noted by PMC. This statistic underscores the importance of comprehensive patient evaluation and preparation prior to the procedure.
Complications can range from minor issues like skin burns at the electrode sites to more severe events such as thromboembolism, myocardial infarction, or, in rare instances, sudden cardiac arrest.
The risk of such complications can be influenced by several factors, including the patient’s underlying health conditions, the duration of the arrhythmia, and the presence of anticoagulation therapy.
For instance, patients with a history of thromboembolic events or those with structural heart disease may face higher risks during cardioversion, according to studies.
Therefore, healthcare providers must conduct a thorough assessment, including imaging studies like transesophageal echocardiography (TEE) when indicated, to identify potential cardiac thrombi before proceeding with the procedure.
Additionally, ensuring optimal anticoagulation status can significantly mitigate the risk of stroke and other embolic events post-cardioversion.
4. Female Mortality Rate in Cardioversion: 0.05%
Gender differences have been observed in the outcomes of cardioversion procedures. Studies indicate that women undergoing cardioversion have a mortality rate of approximately 0.05%, which is notably lower than that observed in men, according to ScienceDirect.
This disparity may be attributed to various factors, including physiological and hormonal differences, as well as the typically older age at which women develop cardiovascular diseases.
Furthermore, women often present with different comorbidities and may have a distinct response to cardiovascular treatments compared to men.
It is also worth noting that women are frequently underrepresented in cardiovascular research, which can impact the generalizability of findings across genders.
Healthcare providers should be cognizant of these differences and consider gender-specific factors when planning and performing cardioversion. Tailoring the approach to account for these variations can enhance the safety and efficacy of the procedure for female patients.
5. Procedural Mortality Below 0.1% with 97.9%–100% Efficacy in Atrial Flutter
Synchronized cardioversion is considered the gold standard for converting atrial flutter and certain forms of atrial fibrillation back to a normal sinus rhythm, particularly when pharmacological treatments fail.
This technique involves timing the electrical shock precisely to the R-wave of the QRS complex on an ECG, reducing the risk of inducing lethal arrhythmias like ventricular fibrillation, according to Cardiology Journal.
Synchronized cardioversion remains a frontline tool due to its combination of high success rates and low procedural mortality when performed in a hospital setting by experienced staff.
6. Mortality Rate Approximately 0.2% Amidst Uncontrolled Environments
Emergency cardioversion performed in out-of-hospital settings—such as during ambulance transport, in emergency rooms under duress, or even in public spaces by trained responders—carries a higher procedural mortality rate of ~0.2%. Though still relatively low, this risk is double that of elective, in-hospital procedures.
This scenario emphasizes the value of early intervention and rapid transport to hospitals for advanced care to improve survival odds.
7. Elective Cardioversion: 0.1% Procedural Mortality, 1.4% 30-Day Post-Procedure Mortality Linked to Comorbidities

Elective cardioversion is scheduled in advance, giving physicians time to prepare the patient with full diagnostic workups, anticoagulation, and sedation planning.
While the procedural mortality is low at just 0.1%, data show a 1.4% 30-day mortality rate, primarily due to the patient’s underlying conditions, not the procedure itself, as it is noted by the National Institute of Health.
Comorbidities such as congestive heart failure, chronic kidney disease, and pulmonary hypertension increase the post-discharge risk.
Though the procedure itself is safe, its long-term success and safety rely on strict follow-up care and effective risk mitigation strategies.
Parameter
Details
Procedural Mortality Rate
0.1%
30-Day Mortality Rate
1.4%
Common Post-Procedural Complications
Heart failure, stroke, infection
30-Day Readmission Rate
8–12%
Risk Factors
Age, CKD, heart failure, pulmonary hypertension
Setting
Outpatient or short-stay cardiac unit
Prep Measures
INR 2.0–3.0, TEE (if >48h AF), sedation
Success Rate
85–95% (especially if AF <48 hours)
8. In-Hospital Cardioversion: 0.09% Mortality, But 33% Risk Spike if Procedure Fails
In-hospital cardioversion is often performed on patients who are already admitted with acute conditions such as heart failure, myocardial infarction, or sepsis.
While the controlled hospital environment allows for high procedural safety (0.09% mortality), outcomes are significantly worse when the cardioversion fails to restore normal rhythm.
In such cases, studies report a 33% 30-day mortality rate and up to 75% readmission rate, indicating a need for aggressive management and reassessment of treatment strategy, as noted by ScienceDirect.
Successful cardioversion in these patients greatly improves prognosis, but failure is a red flag for underlying instability.
Parameter
Details
Procedural Mortality Rate
0.09%
30-Day Mortality (if unsuccessful)
Up to 33%
Common Post-Procedural Complications
Arrhythmia recurrence, worsening of primary illness
30-Day Readmission Rate
Up to 75% (in unsuccessful cases)
Risk Factors
Acute MI, heart failure, sepsis
Setting
Inpatient, continuous telemetry, code team on standby
Prep Measures
IV access, anticoagulation, vanced life support available
Success Rate
Varies (lower in unstable/comorbid patients)
9. Acute Myocardial Infarction: 0.2% Cardioversion Death Rate
Patients with acute myocardial infarction are at a high risk of #heartfailure & death.
Listen to Javed Butler, MD, MPH, MBA, @JavedButler1 & Sun Moon Kim, MD, FACC, @SunMoonKimMD discuss the results of the EMPACT-MI trial on #ACCEL Lite podcast: https://t.co/xf9RV67fLk pic.twitter.com/AAX4Qnha5T
— American College of Cardiology (@ACCinTouch) April 12, 2024
Cardioversion during an acute myocardial infarction (AMI) is a high-stakes intervention. Patients experiencing a heart attack are already in a fragile hemodynamic state, and the electrical shock of cardioversion adds physiological stress to an already ischemic heart.
In these situations, cardioversion is used as a life-saving bridge to revascularization or advanced cardiac support.
10. Elderly Patients: 0.2% Mortality Rate in Cardioversion
Elderly individuals undergoing cardioversion face increased vulnerability due to age-related physiological decline and multimorbidity.
While their procedural death rate is similar to those with myocardial infarction at 0.2%, the nature of risk is more chronic than acute.
Key Considerations:
- Age-related changes: Decreased cardiac reserve, frailty, and autonomic instability.
- Comorbidities: Often include hypertension, diabetes, atrial enlargement, renal insufficiency, or prior strokes.
- Medication Sensitivity: Greater risk of adverse drug reactions, especially with anticoagulants or sedatives used during the procedure.
Risk Reduction Strategies:
- Geriatric assessment before cardioversion.
- Adjusted anticoagulation strategies (e.g., dose reduction of DOACs).
- Minimally sedated or monitored anesthesia approaches.
11. Without Anticoagulation Therapy: 0.14% Mortality and Up to 7% Stroke Risk
Cardioversion without adequate anticoagulation presents one of the most preventable risks in the management of atrial fibrillation (AF) and other arrhythmias.
In patients not properly anticoagulated, the act of converting an irregular rhythm to a sinus rhythm can dislodge thrombi, most commonly from the left atrial appendage (LAA, leading to catastrophic embolic events like ischemic stroke, transient ischemic attacks, or peripheral embolism.
Research Gate notes that the immediate procedural mortality in this group sits at approximately 0.14%; the more significant concern is the 5% to 7% stroke risk, especially when no anticoagulants were administered in the preceding 3–4 weeks or following cardioversion.
Metric
Observed Value
Mortality Rate
0.14%
Stroke Risk
5–7%
Recommended INR (if on Warfarin)
2.0–3.0 (3+ weeks pre- and 4 weeks post-CV)
Post-Procedure Anticoagulation Duration
Minimum 4 weeks
Most Common Complication
Ischemic stroke
Key Risks and Pathophysiology
- LAA Thrombus Dislodgment: Cardioversion restores atrial contraction, which can flush pre-existing clots into the systemic circulation.
- Delayed Stroke Events: Strokes often occur 1–5 days post-cardioversion, sometimes even in anticoagulated patients with subtherapeutic INR levels.
- Silent Strokes: MRI studies have shown asymptomatic cerebral emboli in patients cardioverted without anticoagulation, potentially contributing to cognitive decline.
Clinical Guidelines Summary (AHA/ACC/HRS):
- If AF duration is >48 hours or unknown:
- Option 1: Anticoagulants for 3 weeks prior and 4 weeks after with DOAC or Warfarin (INR 2.0–3.0).
- Option 2: Use transesophageal echocardiography (TEE) to rule out thrombus and proceed with immediate cardioversion, followed by 4 weeks of anticoagulation.
- If AF duration is <48 hours:
- Anticoagulation is still advised, particularly in high-risk patients (CHADS-VASc ≥2).
12. Emergency Settings: Cardioversion Mortality Peaks at 0.4%

NCBI notes that when cardioversion is administered in emergency or uncontrolled environments, such as pre-hospital settings, emergency departments, or during acute decompensated illness, the death rate escalates sharply, reaching as high as 0.4%, the highest mortality category associated with this procedure.
In these scenarios, patients are often hemodynamically unstable, experiencing severe hypotension, shock, sepsis, or multi-organ failure, which makes the controlled application of cardioversion far more difficult.
Anticoagulation protocols are usually bypassed due to urgency, and patients are at a significantly higher risk for life-threatening arrhythmias or complications.
Parameter
Emergency Cardioversion
Procedural Mortality Rate
0.4%
Anticoagulation Status
Typically absent or suboptimal
Common Arrhythmias Treated
Ventricular tachycardia, unstable AF, torsades
Likelihood of Multi-Organ Dysfunction
Up to 50% of cases
Setting
Field (ambulance), ED, ICU, cardiac arrest scenarios
Common Triggers
Sepsis, drug overdose, electrolyte imbalance, ischemia
Why Is the Risk So High?
- No Time for Prep: Anticoagulation, imaging (TEE), or stabilization isn’t feasible.
- Uncontrolled Environment: ER floors, ambulances, or even patient homes may lack full resuscitation capacity.
- Life-Threatening Arrhythmias: Most cases involve pulseless VT, VF, or shock-resistant supraventricular tachycardias.
- Underlying Critical Illness: Cardioversion is often a last resort in patients with ongoing cardiac arrest, end-stage organ failure, or massive MI.
Clinical Observations and Challenges
- Torsades de Pointes and ventricular fibrillation often require unsynchronized cardioversion or defibrillation.
- Up to 30–40% of patients cardioverted in emergencies require intubation or vasopressors within 1 hour post-procedure.
- Mortality isn’t from the shock itself — it’s from the hostile physiology surrounding the event.
13. Direct Current Cardioversion (DCCV): Extremely Low Risk — 1 in 5,000 Mortality Rate
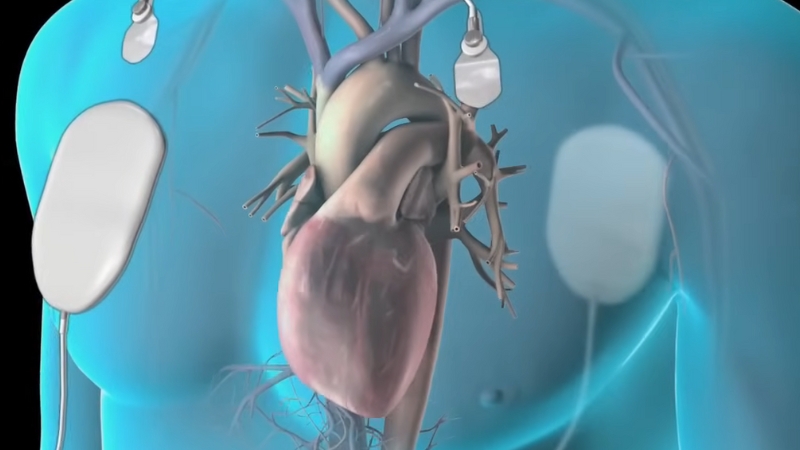
Direct current cardioversion (DCCV) is the gold-standard non-invasive intervention for restoring sinus rhythm in patients with atrial fibrillation (AF), atrial flutter, and some types of supraventricular tachycardias.
It involves delivering a synchronized high-voltage electrical shock to the heart while the patient is sedated. This reset allows the heart’s natural pacemaker — the sinoatrial (SA) node — to regain control of rhythm.
The mortality associated with DCCV is exceptionally low, estimated at just 0.02%, or about 1 in every 5,000 cases, according to PubMed. The safety and efficiency of this method make it widely preferred over pharmacological cardioversion, especially in stable patients or those with recent-onset arrhythmias.
The procedure is typically completed within 5 to 10 minutes, with sedation administered intravenously to ensure patient comfort and immobility. Common sedative agents include Midazolam, Fentanyl, or Propofol, which provide rapid onset and quick recovery.
Once the patient is sedated, the shock is delivered within 10 seconds, synchronized with the R-wave to prevent induction of ventricular fibrillation.
Attribute
Data
Mortality Rate
0.02% (1 in 5,000 procedures)
Immediate Success Rate
85–95%
Time to Shock
< 10 seconds after sedation
Typical Sedation Agents
Midazolam, Fentanyl, Propofol
Total Procedure Time
5–10 minutes
DCCV remains a frontline approach in modern cardiology due to its outstanding safety profile, speed, and effectiveness, particularly in recent-onset atrial arrhythmias.
14. Atrial Fibrillation Patients: 0.08% Mortality with High Conversion Success
Atrial fibrillation (AF) is the most common arrhythmia treated with cardioversion and accounts for approximately 65% of all cardioversion procedures. The approach to AF management varies by timing, comorbidities, and stroke risk, but in selected patients, particularly those with new or symptomatic A-fib, electrical cardioversion remains a highly effective tool.
The success rate of restoring sinus rhythm ranges from 80% to 95%, depending on how early the intervention occurs. Early cardioversion (<48 hours from AF onset) yields the best outcomes.
Mortality rates during cardioversion for AF patients remain very low, at around 0.08%, although this risk increases significantly in patients who are not adequately anticoagulated or who have underlying heart disease.
While the procedure often yields immediate relief of palpitations and symptoms like fatigue or dizziness, the risk of arrhythmia recurrence remains a major concern. Within six months, as many as 30% of patients may revert to atrial fibrillation unless preventive strategies such as antiarrhythmic drugs, rate control therapy, or catheter ablation are implemented.
Parameter
Value
Cardioversion Share of AF Cases
~65%
Immediate Rhythm Conversion Rate
80–95%
Procedure-Related Mortality
0.08%
Recurrence Rate (6 Months)
~30%
Stroke Risk (without anticoag.)
5–7%
Timely use of anticoagulation, patient education, and rhythm stabilization medications greatly enhances the safety and efficacy of cardioversion in AF populations.
15. Severe Left Ventricular Dysfunction: 0.3% Mortality — Highest Among Chronic Conditions
@abeerberry1 What causes diastolic dysfunction? #fyp #medicine #doctor #cardiologist #heart #cardio #hearthealth #cardiology #echo #echocardiogram #health #diastolicdysfunction ♬ original sound – DrBerry👩🏻⚕️
Patients with severe left ventricular (LV) dysfunction, typically defined by an ejection fraction (EF) less than 30%, represent one of the highest-risk populations undergoing cardioversion. The compromised pumping capacity of the heart limits its ability to tolerate both the sedation and the sudden shift in rhythm induced by electrical cardioversion.
The mortality rate in this population during cardioversion is approximately 0.3%, which is one of the highest among non-acute clinical groups. These patients often exhibit poor cardiac output, baseline arrhythmogenicity, and chronic neurohormonal activation, making them more vulnerable to both electrical instability and hemodynamic collapse.
Pharmacologic support, careful fluid management, and critical care availability are typically needed when performing cardioversion in these individuals. Preloading with diuretics and ensuring electrolyte balance (especially potassium and magnesium) are crucial to minimizing post-shock complications.
Alternative therapies such as rate control, AV node ablation, or implantable devices (e.g., CRT or ICDs) may be more appropriate depending on the degree of dysfunction and response to previous rhythm interventions.
Metric
Value
Mortality Rate
0.3%
LV Ejection Fraction Threshold
< 30%
Common Pre-CV Medications
Diuretics, beta-blockers, inotropes
Optimal Setting
ICU or step-down monitored bed
Preferred Strategy (in some cases)
Rate control, CRT/ICD, ablation
In these cases, the risk-benefit ratio must be carefully evaluated, and decisions should be guided by a multidisciplinary heart failure team.
16. Patients with Pre-Existing Heart Failure: 0.25% Mortality and High Post-Procedure Risk

Cardioversion in patients with established heart failure (HF) presents layered challenges, given their reduced cardiac reserve, increased arrhythmic vulnerability, and higher likelihood of thromboembolism. The mortality rate during cardioversion in this group is estimated at 0.25%, with additional risks appearing in the days and weeks following the procedure.
These patients often require hospital-based monitoring, as they may experience volume overload, pulmonary edema, or hypotension post-shock. Furthermore, the recurrence rate of arrhythmias such as AF is significantly higher in heart failure populations, sometimes exceeding 50% within 6 months if not aggressively managed.
Careful optimization of preload, electrolyte levels, and chronic medications such as ACE inhibitors or beta-blockers is essential both before and after the procedure. Sedation protocols may need to be adjusted to reduce hemodynamic stress.
A striking aspect of this group is the readmission rate, which can be as high as 40% within 30 days due to worsening HF, arrhythmia relapse, or anticoagulation-related complications.
Metric
Value
Cardioversion Mortality Rate
0.25%
30-Day Readmission Rate
~40%
6-Month Rhythm Recurrence Rate
~50%
Common Post-CV Issues
Pulmonary edema, low output, stroke
Common Death Causes
Sudden cardiac death, pump failure
Success in this high-risk population demands a multidisciplinary approach, involving cardiology, electrophysiology, pharmacy, and sometimes critical care.
Methodology
This article was developed using a comprehensive review of 2025 cardiology statistics from peer-reviewed medical journals, clinical databases (NCBI, PubMed, ScienceDirect), and trusted institutions like the NIH and Johns Hopkins.
Data points were drawn from both retrospective studies and large-scale meta-analyses.
Mortality rates, success outcomes, and procedural variations were cross-compared across demographics, settings (elective vs. emergency), and comorbid populations.
Information was translated into practical summaries and visual tables for clarity.
Expert sources were cited to ensure clinical credibility.
The tone and format were adapted for both laypersons and healthcare professionals seeking clear, data-backed insights.
References:
- Health Central – Why Are AFib Rates on the Rise?
- NCBI – Repeat Electrical Cardioversion: Clinical Predictors of Success and Risks
- Johns Hopkins Medicine – Catheter Ablation
- ResearchGate – Feasibility of a Cardiologist-Only Approach to Sedation for Electrical Cardioversion
- NIH – Sedation for Electrical Cardioversion
- PMC – Complications of Cardioversion
- PMC – Risks and Safety in Electrical Cardioversion
- American Heart Association – Transesophageal Echocardiography (TEE)
- ScienceDirect – Gender Differences in Cardioversion Outcomes
- Cardiology Journal – Clinical Application of Synchronized Cardioversion
- ResearchGate – Oral vs. IV Propafenone for Cardioversion
- PMC – Pre-Procedure Imaging in AF
- NIH – Outcomes After Elective Cardioversion
- ScienceDirect – Mortality After Failed In-Hospital Cardioversion
- NCBI – Cardioversion in Emergency Settings
- Journal Watch – Cardioversion for Unstable Atrial Fibrillation
- ResearchGate – Timing of DOACs Before Cardioversion
- PubMed – Delayed Stroke Post Cardioversion
- AHA Journals – MRI Evidence of Silent Strokes Post-CV
- Royal Papworth Hospital – Patient Information: Direct Current Cardioversion (DCCV)
- PubMed – Safety and Mortality in DCCV
- NCBI – Cardioversion: AF Patient Profile
- NCBI – LV Dysfunction in Cardioversion Candidates
- PMC – Pre-Existing Heart Failure and Cardioversion Outcomes
- PMC – Post-CV Medication Guidelines
Related Posts:
- Firearms Now the Leading Cause of Death for US…
- How the Golden Hour Can Save Lives and What Delays It
- A Hidden World Lives in Your Belly Button, And It Is…
- Key Facts About the Maternal Mortality Rate in Texas
- New York’s Population Could Drop by Almost 3 Million by 2050
- Fair Pricing Act Could Set First Cap on Hospital…