In the United States, over 85% of seniors aged 65 and older live with at least one chronic condition, and more than half manage two or more.
These conditions—ranging from cardiovascular disease and diabetes to arthritis and chronic obstructive pulmonary disease (COPD)—significantly impact seniors’ quality of life, independence, and longevity.
In 2022 alone, chronic respiratory diseases—including COPD—accounted for 147,382 deaths in the United States, with the condition affecting 11.7 million adults.
Similarly, diseases like diabetes and hypertension not only reduce the quality of life but also exacerbate the risk of complications such as cardiovascular events and cognitive decline.
Depression, chronic pain, and sleep disorders further compound these challenges, often interacting with physical conditions to intensify their effects.
Table of Contents
Toggle1. Over 85% of Seniors Have at Least One Chronic Condition
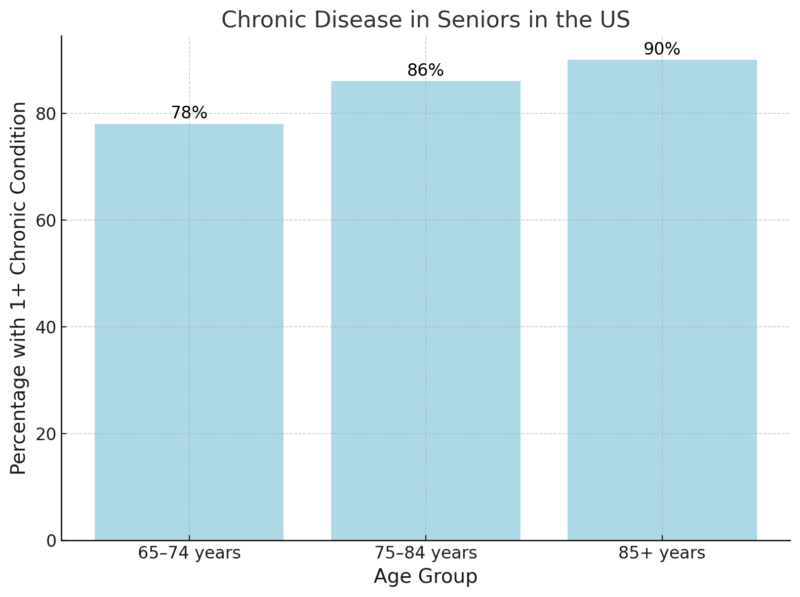
85% of adults aged 65 and older live with at least one chronic disease according to an NIH study.
Chronic diseases such as hypertension, arthritis, and diabetes are pervasive among older adults, with more than 85% of seniors managing at least one condition.
This prevalence reflects the cumulative impact of aging, where biological changes and prolonged exposure to risk factors such as poor diet, physical inactivity, or smoking contribute to disease development.
The rates increase with age, as shown in the table: nearly 90% of those over 85 have at least one chronic disease compared to 78% of those aged 65–74.
These conditions pose substantial public health challenges, requiring sustained medical attention and often leading to functional limitations or dependency on caregivers.
2. 56% Have Two or More Chronic Conditions
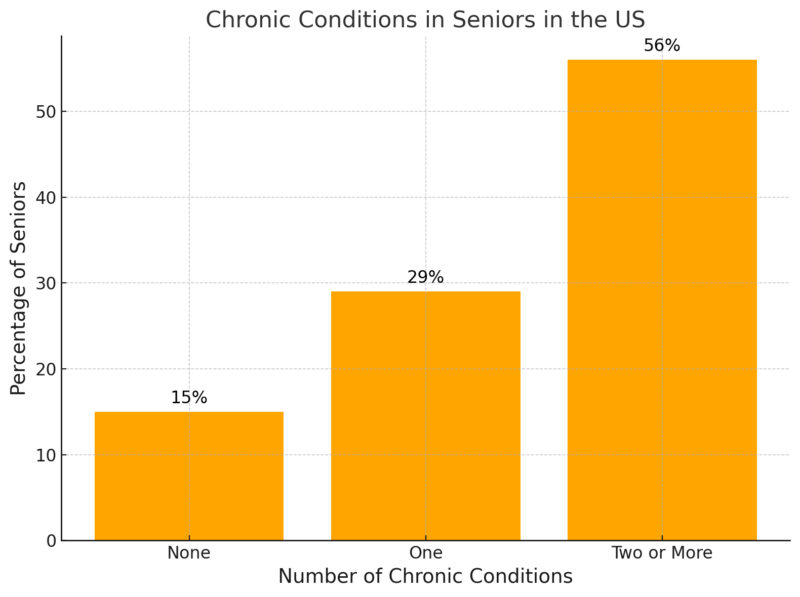
NCBI notes that 56% of seniors are affected by two or more chronic diseases and over half of all seniors face the challenge of managing multiple conditions simultaneously, which complicates medical care.
For instance, treating a patient with both diabetes and cardiovascular disease requires careful coordination to avoid adverse interactions between medications while also addressing overlapping symptoms and risk factors such as high blood pressure or obesity.
The 15% of seniors without chronic conditions often represent individuals with favorable genetics, robust preventive healthcare, and healthier lifestyles. However, the majority of seniors require frequent engagement with healthcare systems to manage their conditions.
Multimorbidity is associated with higher hospitalization rates, longer hospital stays, and increased healthcare expenditures.
3. Cardiovascular Disease Affects Over 44% of Seniors
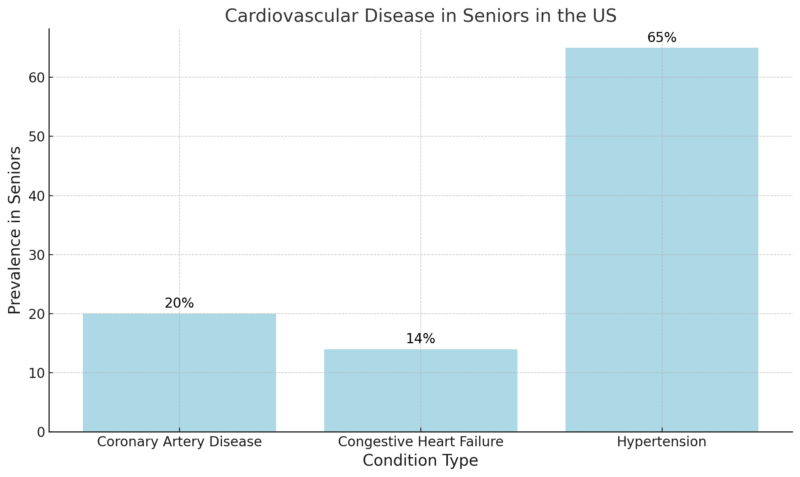
44% of men and 46% of women aged 65+ have been diagnosed with some form of cardiovascular disease according to CDC report.
Cardiovascular disease (CVD) is one of the leading causes of morbidity and mortality among seniors, affecting nearly half of this population.
Hypertension, which affects 65% of seniors, is often a precursor to more severe conditions such as coronary artery disease and congestive heart failure.
The prevalence of coronary artery disease (20%) and heart failure (14%) underscores the high cardiovascular burden in this demographic.
Age-related changes, such as stiffening of blood vessels and declining cardiac efficiency, contribute to increased susceptibility to CVD.
Hypertension often develops silently over decades and leads to long-term damage to blood vessels and organs.
4. Diabetes Impacts 28% of Seniors
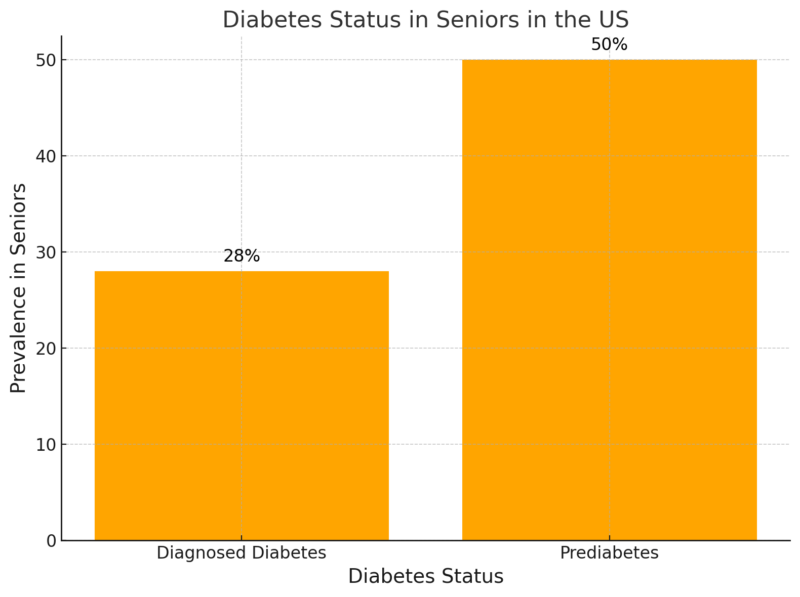
JAMA research notes that 28% of seniors live with diabetes, while 50% have prediabetes.
Diabetes is a major health challenge for seniors, with nearly 1 in 3 diagnosed and another 50% at risk due to prediabetes.
Seniors with diabetes face a higher risk of hospitalization and complications during medical procedures compared to their non-diabetic peers.
The 50% prevalence of prediabetes highlights the urgent need for early intervention to prevent the progression to type 2 diabetes.
Effective diabetes management in seniors requires individualized approaches due to potential challenges such as cognitive decline, mobility issues, or the presence of other chronic conditions.
Regular blood glucose monitoring, adherence to treatment plans, and lifestyle modifications such as increased physical activity and healthier eating habits are critical.
Healthcare systems must prioritize diabetes education and access to resources to help seniors manage their condition and prevent long-term complications.
5. Arthritis Affects 50% of Seniors
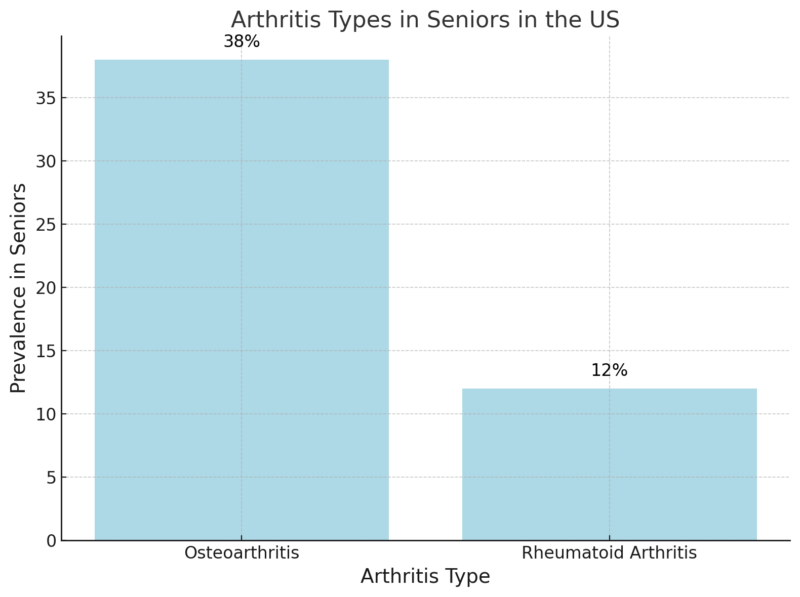
50% of seniors aged 65+ have been diagnosed with arthritis.
Arthritis impacts half of the senior population, significantly limiting mobility and independence.
Richard F Loeser notes that osteoarthritis, the most common form, affects 38% of seniors and is associated with joint wear-and-tear exacerbated by aging and mechanical stress.
Rheumatoid arthritis, though affecting 12%, often has more severe consequences, including joint deformity and chronic pain due to its autoimmune nature.
Both forms of arthritis are major contributors to disability in older adults.
Treatment options focus on symptom management, including medications (e.g., NSAIDs or biologics for rheumatoid arthritis), physical therapy, and, in severe cases, joint replacement surgeries.
6. 20% of Seniors Have Chronic Obstructive Pulmonary Disease (COPD)
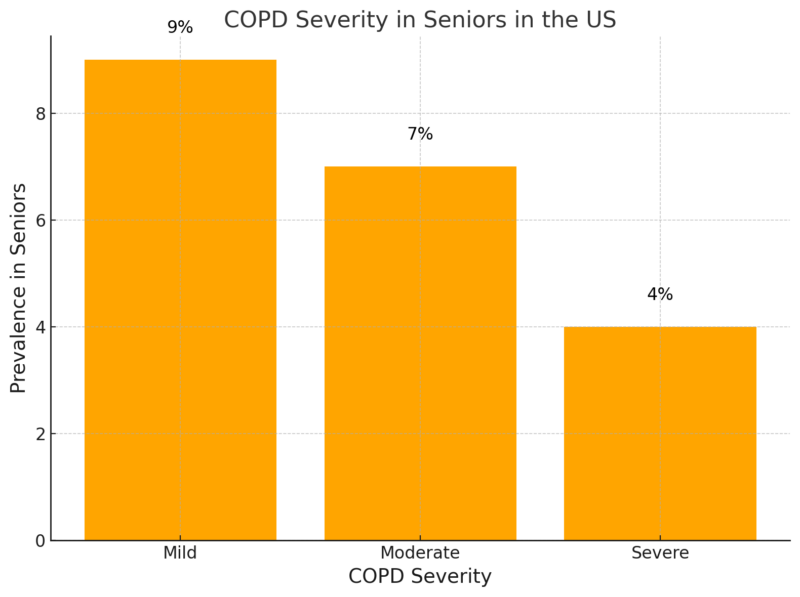
COPD is a progressive and often debilitating lung condition that impacts 20% of seniors, with varying degrees of severity according to Statista.
Mild cases, affecting 9%, may only require occasional bronchodilator use and lifestyle adjustments, while moderate to severe cases (11% combined) often necessitate advanced interventions, including oxygen therapy and pulmonary rehabilitation.
Smoking remains the leading cause of COPD, although environmental exposures and genetic predispositions also play significant roles. The economic burden of COPD includes increased hospitalizations, frequent use of emergency care, and long-term disability.
Interventions such as smoking cessation programs and access to early pulmonary function testing are essential to slow disease progression and improve life expectancy.
7. Depression Affects 15% of Seniors
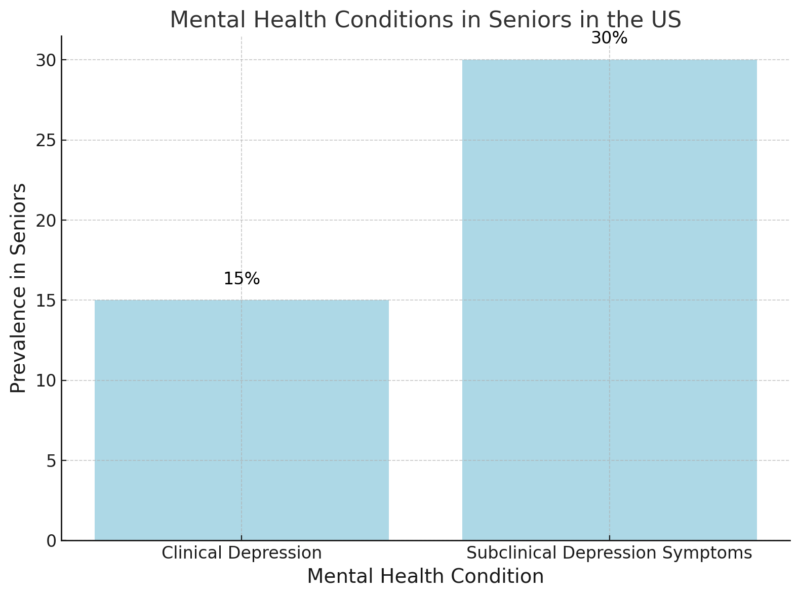
Amy Fiske the researcher from PMC NCBI noted in the study that depression in seniors is both prevalent and underdiagnosed, with 15% experiencing clinical depression and up to 30% showing subclinical symptoms such as persistent sadness or low energy.
This mental health issue is often exacerbated by chronic diseases, social isolation, and bereavement, which are common in this age group.
Depression is not a normal part of aging; however, it can be common in #OlderAdults. Depression can affect how a person feels, acts, and thinks. Learn more about #depression and older adults with this infographic: https://t.co/zojZ3pWTbd #MentalHealthAwareness #MHAM2024 pic.twitter.com/OnyX9XOBp9
— The National Institute on Aging (NIA) (@NIHAging) May 7, 2024
Untreated depression can lead to worsening physical health, higher mortality rates, and diminished quality of life. Integrating mental health assessments into routine care is critical. Treatment options, including psychotherapy and antidepressant medications, can significantly improve outcomes.
8. 25% of Seniors Experience Chronic Pain
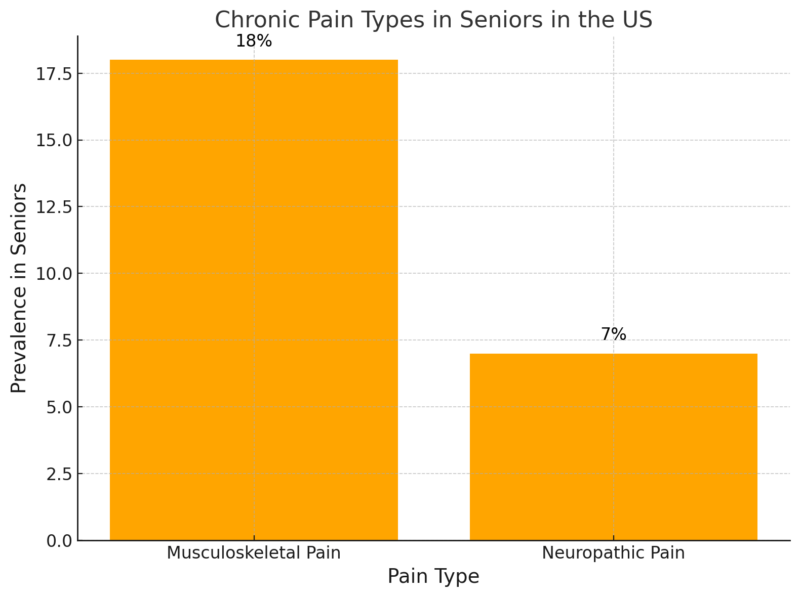
1 in 4 seniors reports experiencing chronic pain, often related to conditions like arthritis or neuropathy.
Chronic pain affects 25% of seniors, with musculoskeletal pain (18%) and neuropathic pain (7%) being the most common types.
Chronic pain is often linked to underlying conditions such as arthritis, osteoporosis, or diabetic neuropathy, and it significantly impacts mobility, mood, and daily functioning.
Effective pain management for seniors is complex due to the potential for drug interactions and the risks associated with long-term opioid use. Non-pharmacological interventions, such as physical therapy, acupuncture, and cognitive-behavioral therapy, are increasingly recognized as vital components of a comprehensive pain management plan.
9. Cognitive Decline Affects 11% of Seniors
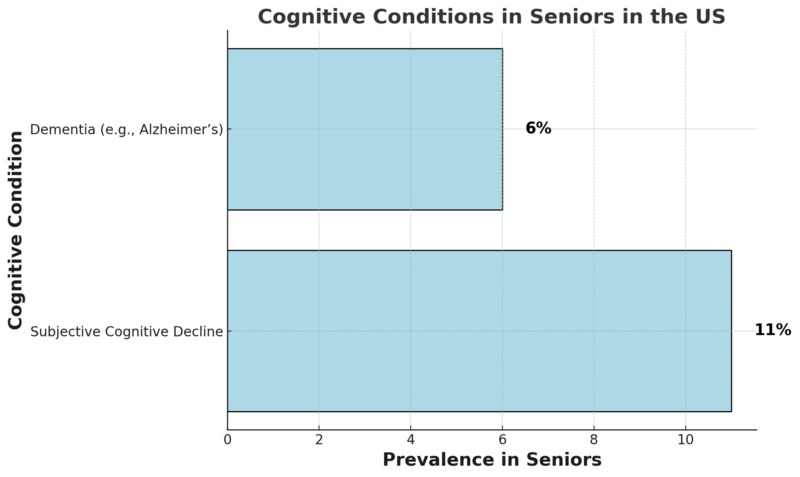
Cognitive decline impacts 11% of seniors, with 6% experiencing dementia-related conditions like Alzheimer’s disease.
Subjective cognitive decline is often an early warning sign of more serious conditions and warrants further evaluation.
These conditions not only reduce independence but also place significant emotional and financial burdens on families and caregivers.
Interventions such as cognitive training, dietary modifications, and regular physical activity may help slow cognitive decline.
Additionally, early detection programs and memory clinics can aid in managing symptoms and planning for care.
10. 35% of Seniors Have Sleep Disorders
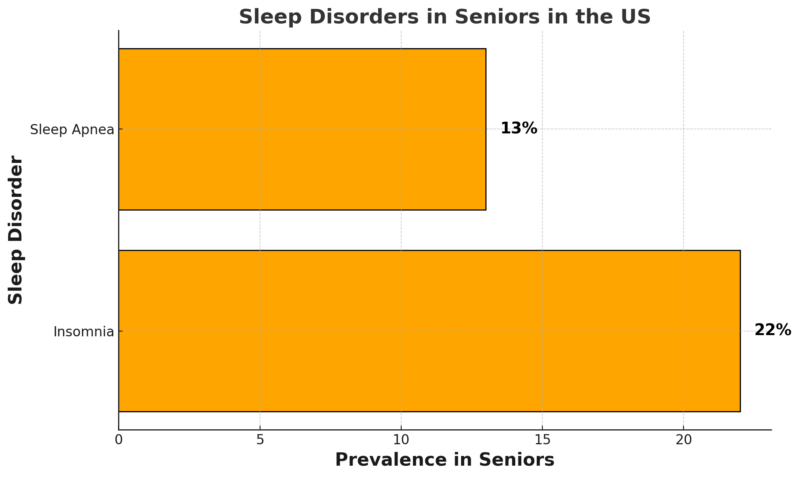
Sleep disorders affect more than a third of seniors, with insomnia (22%) and sleep apnea (13%) being the most common.
Poor sleep quality is associated with increased risks of chronic conditions such as hypertension, diabetes, and depression. Sleep apnea, in particular, is linked to cardiovascular disease due to repeated interruptions in oxygen supply during sleep.
Treating sleep disorders requires a multifaceted approach.
PubMed notes that for insomnia, cognitive-behavioral therapy and sleep hygiene education are effective, while CPAP (continuous positive airway pressure) devices are the gold standard for managing sleep apnea.
Methodology
This article was crafted using a comprehensive review of peer-reviewed journals, government health databases, and reputable medical resources such as NIH, CDC, JAMA, and PubMed.
Key statistics were sourced directly from credible studies and reports to ensure accuracy and relevance.
Data was analyzed to highlight the prevalence and impact of chronic diseases on seniors, focusing on trends and actionable insights.
Tables were included to visually present complex data for better comprehension.
The article integrates expert commentary and research findings to provide a well-rounded perspective on each condition.
All information was synthesized to create an informative yet accessible resource for readers interested in senior health.
References:
- NIH – 85% of Americans Over 65 Live with At Least One Chronic Condition
- NCBI – Multimorbidity Among Older Adults: Prevalence and Implications
- CDC – Women and Heart Disease
- JAMA – Prevalence of Diabetes and Prediabetes Among Older Adults
- Richard F. Loeser – Aging and Osteoarthritis
- PMC NCBI – Rheumatoid Arthritis Prevalence in Seniors
- Statista – COPD, Emphysema, or Chronic Bronchitis Prevalence Among Seniors in the U.S.
- PMC NCBI – Depression in Seniors
- PMC NCBI – Chronic Pain Management in Seniors
Related Posts:
- 10 Shocking Statistics About Heart Disease in 2025
- Idaho Population Growth in 2025 - Everything You…
- 2025 HSA Contribution Limits - What You Need to Know
- El Paso Population 2025 - What You Need To Know
- Population Data for Rhode Island 2025 - What You…
- Arkansas’ Population in 2025 - Everything You Need to Know