When Medicaid expansion rolled out under the Affordable Care Act, it was a game-changer. Millions of low-income Americans, many for the first time in their lives, finally had health coverage. More check-ups, more prescriptions filled, more conditions caught early, that’s the good part.
But here’s the flip side: emergency rooms have gotten a whole lot busier. And not just with critical cases. Since the expansion, ERs across the country have seen longer wait times, more patients walking out before being seen, and a growing strain on already maxed-out hospital staff.
So, has Medicaid expansion made ER overcrowding worse? Short answer: yes.
Not because the coverage itself is bad, but it’s necessary. But because the infrastructure around it hasn’t kept up. More people have coverage, but many still can’t find a primary care doctor or get into a clinic when they need to. So they turn to the emergency room, even when it’s not truly an emergency.
The result? Overcrowded ERs, delayed care, and rising frustration on all sides.
Table of Contents
ToggleMore Coverage, More Crowding
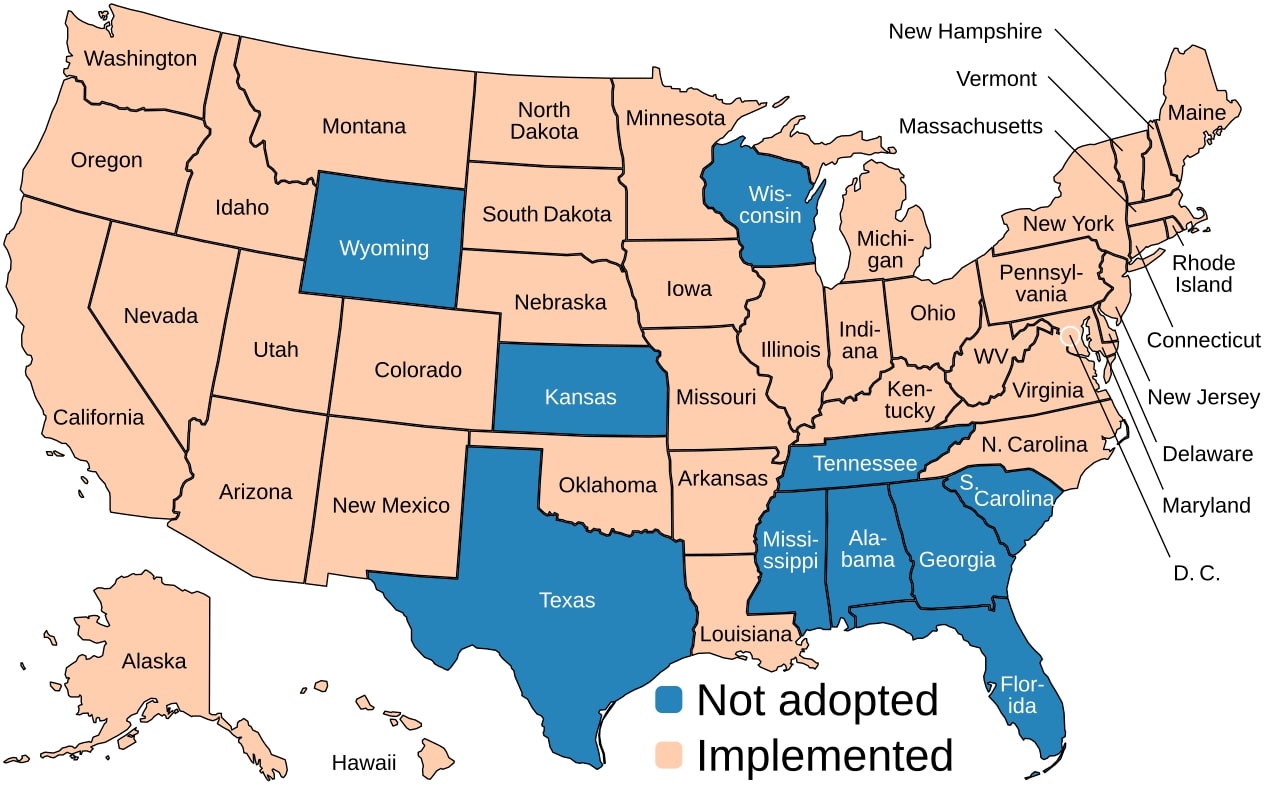
Back in 2010, the Affordable Care Act (ACA) gave states the option to expand Medicaid to low-income adults who previously didn’t qualify. Over 40 states have now done it in some form, according to KFF. The goal?
Give more people coverage. Fewer people falling through the cracks. It was a big, bold move, and by most measures, it worked.
But here’s where things started getting sticky.
When states expanded Medicaid, more people were able to seek care. That sounds great, right? Except many of them didn’t have regular doctors. Or couldn’t find one. So where did they go?
The emergency room.
Now, don’t get me wrong, ERs are critical. They save lives. But they’re not designed to be the front door of the healthcare system. They’re expensive, high-stakes environments. And when more people start treating them like urgent care centers or primary care offices, the system buckles.
And the numbers back it up:
Changes in ED Wait Times and Patient Behavior

| Metric | Pre-Expansion | Post-Expansion | Percentage Change |
| Average Wait Time to See Provider (minutes) | 30.8 | 34.3 | +11.4% |
| Patients Leaving Without Being Seen (%) | 2.5 | 2.9 | +16% |
What you’re seeing here is more than just a few extra minutes. A nearly 11.5% jump in average wait time adds up fast in a busy ER. For hospitals that already had limited beds and overworked staff, this has made a chaotic environment even harder to manage.
And that 16% spike in patients leaving without being seen? That’s a red flag. It means people are giving up and walking out – either out of frustration or because they just can’t wait anymore. In some cases, that delay could be dangerous.
A Look at the Numbers
Let’s pull back the curtain with some actual stats:
- In states that expanded Medicaid, wait times to see an emergency room provider went up by about 10%.
- The percentage of people who gave up and left before being seen jumped by 15%.
- “Boarding time” – the delay between being admitted and actually getting a hospital bed – also increased.
These numbers came out of a study published on Research Gate and highlighted by researchers at Northwestern University. It’s not just abstract data, it’s a very real strain on patients and staff.
And while those stats are averages, in some urban hospitals, especially safety-net ones, the effects have been even more dramatic.

Why the Surge?
So, what’s really driving the spike in ER use among people newly covered by Medicaid?
Turns out, there are a few overlapping reasons. Let’s break it down:
1. Hard Time Finding Primary Care
Here’s the blunt truth: having Medicaid doesn’t mean every doctor will see you. Medicaid pays doctors less than private insurance, and many providers are already maxed out.
Especially in areas with fewer clinics or fewer doctors per capita (think rural Appalachia, parts of the South, and even some urban centers), Medicaid patients can struggle to find someone willing – or able – to take them.
So when your kid has an ear infection, or you need a medication refill, the ER starts to feel like the only option.
2. Regional Healthcare Deserts
In rural places – like where a lot of the Amish live, by the way – you might be hours from a proper hospital, and even further from a doctor who sees Medicaid patients. It’s not just about coverage. It’s about geography. When the closest doctor is 40 miles away and doesn’t take your plan, you’re going to end up in the ER when anything goes sideways.
3. Trust, Habit, and Convenience
Sometimes it’s cultural. Some people, especially if they’ve gone years without coverage, don’t have a primary care doctor or a habit of preventative care. They’ve used the ER when something feels urgent – because it’s open, it’s familiar, and no one turns you away.
Others just figure they’ll be seen faster or treated better in the ER than at a busy clinic. And hey, if you’ve ever waited three hours in a community health center waiting room, that logic checks out.
The Oregon Case Study: What Happened When Medicaid Expanded Overnight
Let’s zoom in on Oregon for a second. Back in 2008, before the ACA even passed, Oregon ran a sort of natural experiment. They had enough funding to expand Medicaid to a limited number of low-income adults, so they ran a lottery. Some got coverage. Others didn’t.
Turns out, those who got Medicaid used the emergency room 40% more than those who didn’t, as noted by NPR. Over 18 months, the spike was spread across all kinds of issues, from urgent to stuff that really could’ve been handled elsewhere.
Now, fast forward to post-ACA. The same trend happened again, but on a bigger scale. California saw a huge rise in ED visits after expansion. So did New York, Colorado, and a long list of others.
More coverage equaled more use. Simple as that.
ED Visit Rates Pre- and Post-Medicaid Expansion
The Oregon story wasn’t just a one-off. States across the map saw similar trends in the years after Medicaid expansion kicked in:
ED Visit Rates Pre- and Post-Medicaid Expansion
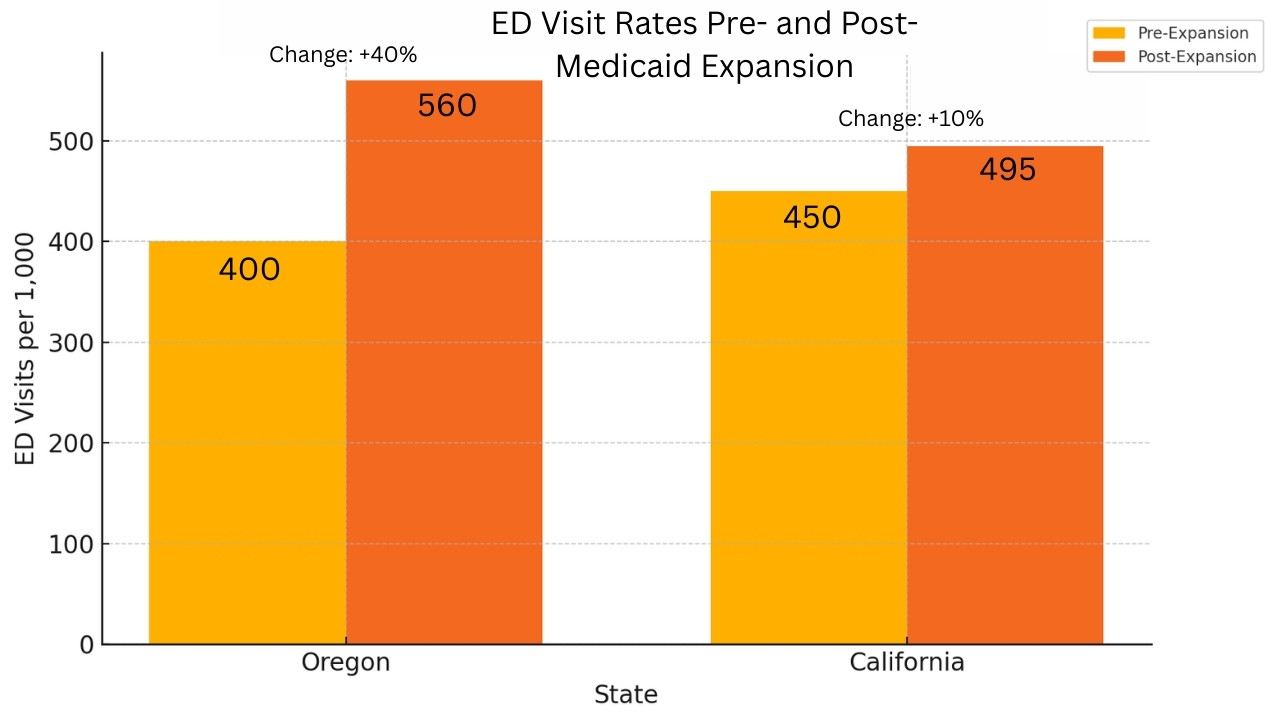
Oregon’s numbers are especially eye-catching, an increase of 160 visits per 1,000 people. That’s a 40% spike, in less than two years. California, though a much larger and more complex system, still saw a solid 10% bump.
These aren’t just abstract percentages, they translate into thousands more people walking into emergency rooms every week. And more often than not, they’re not there for true emergencies. They’re there because they can’t find a doctor, or don’t know where else to go.
Not All Bad News: Some ER Visit Rates Are Leveling Off
Before we paint the whole picture in gloom, there’s a twist.
A study from JAMA Network Open suggested that in some places, overall emergency room visits actually dropped a few years after expansion – by about 4.7 visits per 1,000 people. That suggests the spike might be temporary in some areas, tapering off as people figure out where else to go.
Still, that kind of decline isn’t universal. The general trend, especially in the short term, has been up and to the right.
So What’s the Fix?
Let’s be real: this isn’t the fault of people getting insured. It’s a sign that the system around them isn’t quite ready to support them.
So what can we do?
1. Raise Medicaid Reimbursement Rates
If Medicaid paid providers more, more doctors might actually accept it. That means more options for patients, and fewer trips to the ER for non-emergencies. It’s simple economics.
2. Expand Community Health Centers
Especially in rural areas, where doctor shortages are already dire, beefing up federally qualified health centers (FQHCs) could make a huge difference. These clinics take Medicaid and uninsured patients, and they offer wraparound services – mental health, substance use, and preventive care.
3. Educate Patients Without Shaming Them
People don’t go to the ER for fun. Sometimes they don’t know what else to do. Patient education, not finger-wagging, can help steer people to better options. That could be urgent care, telehealth, or 24/7 nurse lines.
Even Amish communities, which often opt out of traditional insurance systems, rely on local clinics and midwives. But when complications arise, even they head to the hospital. It’s all about trust and what’s available.
4. Try Integrated Care Models
Some states and systems are testing new ways to connect Medicaid patients with a single “home” for their healthcare, a place where they see the same doctor regularly and can get labs, prescriptions, and follow-up in one spot.
That continuity matters. It builds trust. It reduces the need to run to the ER every time something feels off.
Bottom Line
Medicaid expansion did what it set out to do: give more people healthcare coverage. But just giving someone a card isn’t enough if the system can’t back it up. When folks can’t find a doctor, or aren’t sure where to turn, they end up in the ER.
That’s not because they’re abusing the system. It’s because the system isn’t quite meeting them halfway.
Fixing ER overcrowding isn’t about reversing expansion. It’s about investing in the parts of healthcare that make expansion work: access, trust, and smart design.
The emergency room should be there for heart attacks, accidents, strokes,not the flu or a refill for blood pressure meds. But until the front doors of healthcare are wide open for everyone, the ER will keep picking up the slack.
And that’s not fair – to patients or to the people working double shifts in trauma bays and triage units trying to hold it all together.








