When I first encountered remote-patient-monitoring (RPM) programs in a cardiology clinic, I thought: this could be the healthcare shift we’ve waited for.
The global RPM market is already worth ~US $22.03 billion in 2024 and is projected to grow to US $110.71 billion by 2033, with a CAGR of 19.8 % between 2025–2033, according to Grand View Research.
That magnitude tells us three things: RPM is no niche pilot any longer; its scale is real; and the potential to influence care delivery is significant.
Table of Contents
ToggleThe Market: Expansion by Necessity
The shift from reactive to preventive care explains the surge. By 2025, chronic illness will affect nearly half of adults in the United States, and hospital readmissions will cost systems tens of billions annually.
For CFOs and policymakers, RPM’s math makes sense, keeps patients home, and saves money.
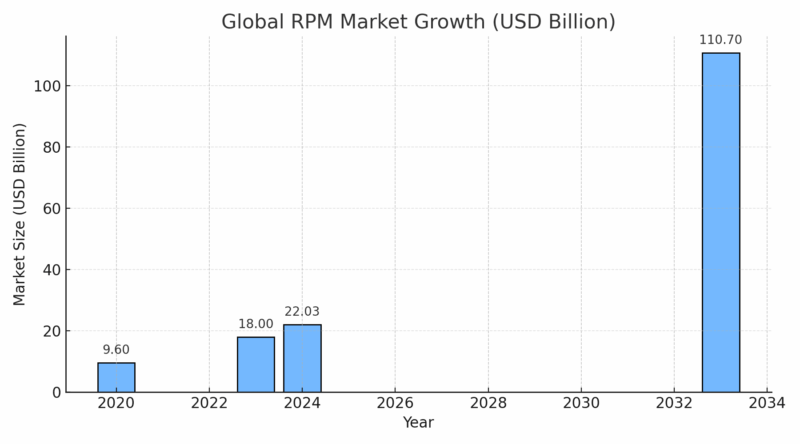
North America still leads with about 40–45 percent of total revenue, but Asia-Pacific is the fastest-rising region, driven by mobile-first health networks.
As Oren Nissim, CEO of Brook Health, put it during a 2024 press briefing:
“This approach combines technology and human expertise to extend the reach of healthcare teams.”
That blend, data plus clinician oversight, defines RPM’s next phase of growth.
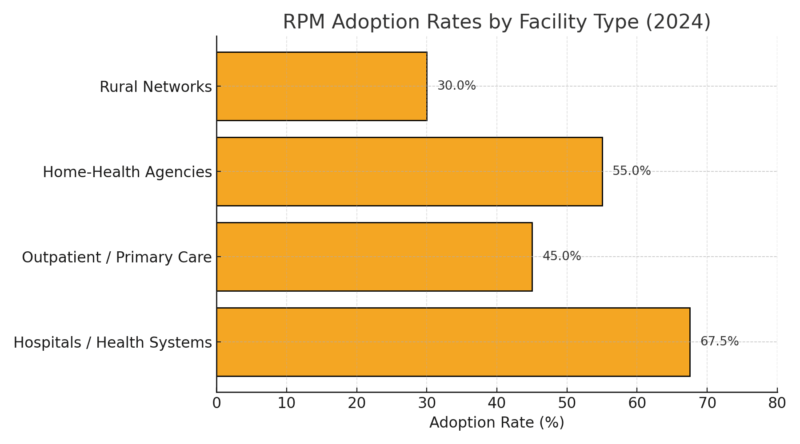
Adoption: From Pilot Program to Default Setting
In 2019, RPM was a billing code that few providers understood. By 2025, it is routine. Medicare claim volumes for RPM codes (99453–99458) increased by more than 3,000 percent in four years.
Hospitals use it to track discharged patients; outpatient clinics use it for hypertension and diabetes; home-health agencies use it to prevent rehospitalization.
Clinicians note that success depends on design. “Patient selection is important on the front end,” said Dr. Neal Sikka of George Washington University. “Who will really benefit, and for what condition?”
It’s a subtle point but crucial. A poorly designed program produces noise; a targeted one delivers savings and safety.
Measured Outcomes: Evidence and Real-World Results
The early promise of RPM is finally backed by consistent data.
Metric
Baseline
With RPM
Change
30-day heart-failure readmissions
18 %
9 %
−50 %
Hospitalizations (per 3 months)
0.45 /patient
0.19 /patient
−58 %
ED visits (per patient)
0.30
0.18
−40 %
Avg. hospital stay
5.6 days
4.1 days
−27 %
The most-cited real-world example remains the UMass Memorial Health program. Its remote-monitoring and care-team model for heart-failure patients cut 30-day readmissions in half. As reported by The American Journal of Managed Care,
“A 50 percent reduction in 30-day readmissions for heart failure using remote monitoring and care teams.”
The mechanics were simple but effective: patients weighed in daily, transmitted vitals via Bluetooth, and pharmacists or nurses followed alerts in real time.
Similar success appeared in hypertension. At a 2024 American Heart Association meeting, researchers from Geisinger reported:
“Up to 74 percent of adults with resistant hypertension achieved control within one year with Bluetooth monitoring plus pharmacist interactions.”, Dr. Alexander Chang
Dr. Wanpen Vongpatanasin of UT Southwestern, who reviewed the findings, summarized them bluntly:
“This team-based model signals a way to reduce hospitalization and improve blood pressure.”
These aren’t isolated anecdotes. Across dozens of studies, RPM’s pattern repeats: earlier interventions, better adherence, lower utilization.
Economics: The Reimbursement Revolution
The single most important policy change in digital health happened quietly: CMS reimbursement parity for remote monitoring. Providers now bill about $38–$48 per month for RPM review, turning what used to be an unfunded pilot into a steady revenue stream.
Forty-plus state Medicaid plans have aligned coverage, and private insurers have followed.
Yet, as AHRQ’s PSNet review noted, success isn’t automatic:
“Billing and payment remain challenges that disincentivize expansion due to upfront costs.”
For smaller practices, equipment and staffing still present entry barriers. But the macro picture is unmistakable: reimbursement transformed the economics from novelty to necessity.
Technology: From Monitoring to Prediction
Five years ago, RPM meant Bluetooth cuffs and PDFs. Today, it’s predictive analytics, cloud APIs, and integrated telehealth platforms that unify data streams in real time.
Technology Trend
Function
Market Effect
IoT integration
Continuous, low-latency data
Broadened home-monitoring reach
AI analytics
Predictive deterioration alerts
Reduced clinician workload
EHR interoperability
Streamlined data transfer
Improved clinical response time
Consumer wearables
Expanded data sources
Bridge between wellness and care
Cloud security compliance
HIPAA / GDPR standards
Core procurement driver
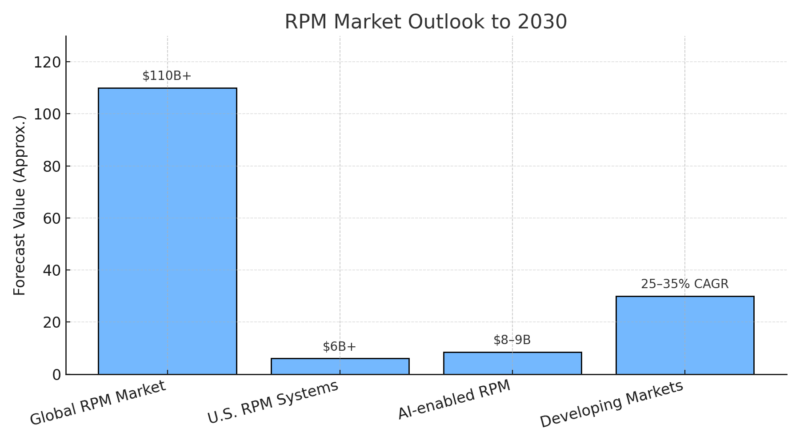
Artificial-intelligence-assisted RPM alone is projected to surpass $8 billion by 2030, as algorithms identify subtle vital-sign deviations before symptoms manifest.
Still, clinicians stress fundamentals. “The most important part of RPM,” said Dr. Colton Hood of GW University, “is good education about devices and what to do concerning readings.”
Technology amplifies care; it doesn’t replace it.
Workflow and Safety: Human Oversight Still Matters

Even the most advanced data pipeline needs people. According to AHRQ PSNet,
“Successful programs have dedicated staff to monitor status and communicate directly with patients.”
Dr. Chandra described how it looks in practice:
“Someone can reach out if any metric is high and advise escalation to a provider.”
That workflow, immediate human follow-up, is what converts remote data into real clinical outcomes. As he added,
“Many good clinical outcomes are the result of education.”
The emphasis on human judgment is why hospitals now treat RPM as an extension of nursing rather than a replacement for it.
The Other Side of the Evidence
Not every trial shows dramatic gains. The EMPOWER Heart Failure study, for instance, found no mortality or readmission improvement after a year of remote monitoring.
It’s a reminder that design quality and engagement levels decide success. Programs without clear escalation paths or patient accountability tend to underperform.
That nuance gives the story credibility: RPM is not a magic fix. It’s a system whose results depend on integration, consistency, and context.
Barriers: Integration, Fatigue, and Equity
Barrier
Impact
Comment
Workflow overload
Alert fatigue, burnout
“Too many numbers, not enough narrative,” one nurse told me.
Reimbursement lag
Slower rural adoption
Delays in payer alignment limit coverage.
Digital divide
Connectivity gaps
Older and low-income populations risk exclusion.
Evidence uniformity
Inconsistent data
Need for standardized outcome reporting.
Physicians I spoke with describe the same tension: RPM produces clarity for patients, but noise for providers.
The next wave of software is trying to fix that: smarter triage, fewer false positives, clearer dashboards.
Outlook to 2030 – Continuous Care Becomes the Default
Every trend line points the same way. The global RPM industry will exceed $100 billion within a decade, with 70–80 percent of large health systems using continuous monitoring for at least one chronic condition.
The software and analytics sub-market will grow even faster, reaching $65 billion by 2030.
As Dr. Vongpatanasin told an AHA panel, “We’re learning that data are only useful when connected to people who act on them.” That line captures the next decade’s challenge perfectly.
Closing Analysis
Remote patient monitoring has crossed its proof-of-concept phase. The market is expanding, outcomes are documented, and policy has caught up.
Yet the defining question remains human: how to design systems that care as efficiently as they measure.
The data show what the future looks like: hospital corridors less crowded, chronic-disease management more precise, clinicians watching risk scores rather than waiting for crises.
But the quotes from those running the programs tell us what matters most: patient trust, education, and timely intervention.
Related Posts:
- Protecting Patient Data – Are Healthcare Providers…
- How America Spends, Shops, and Travels on July 4th -…
- Visitor Volume in Las Vegas by the Numbers - A 2025 Update
- Dental Care in the US: What the Numbers Reveal About…
- How Many Children Are Adopted in the United States -…
- Teen Depression Statistics in the US - A Closer Look…