When an older adult suffers a serious fall, it does not simply count as an accident. It functions as a biological warning signal, an inflection point that often marks the beginning of irreversible decline.
The data is consistent across decades of research: a fall in adults over 65 significantly shortens life expectancy, even more so when the fall results in a hip fracture, traumatic brain injury, vertebral compression fracture, or prolonged immobility, according to URMC.
To state the prognosis plainly:
- Falls are the leading cause of injury-related deaths in Americans 65+.
- The 2023 mortality rate reached 69.9 deaths per 100,000, rising to 373.3 per 100,000 in those 85+, according to the CDC.
- Hip fractures kill up to one-third of patients within a year.
- Traumatic brain injuries from falls carry up to a 32.9% one-year mortality.
- Vertebral fractures raise long-term mortality eightfold.
- Fear of falling itself nearly doubles the risk of death (HR 1.86).
A fall does not merely injure the body. It exposes underlying frailty, accelerates physiological decline, hastens functional disability, and introduces a cascade of complications, from pneumonia to sepsis to the psychological dismantling of independence.
The Epidemiology of an Underestimated Crisis
A Mass-Scale Problem Hidden in Plain Sight
CDC notes that every second in the United States, an older adult falls. That adds up to 14+ million falls annually, affecting around 25%–30% of the entire senior population.
Yet fewer than half report the incident, usually because they fear losing autonomy or being forced into assisted living.
The first fall is more than a warning. It doubles the risk of falling again within the next year. The second fall is often catastrophic: a hip fracture, a subdural hematoma, or a long-lie event that accelerates deadly complications.
The Mortality Gap Across Age, Gender, and Race
Gender Paradox
- Women fall more often (28.9% vs 26.1%).
- Men die more often (74.2 vs 66.3 deaths per 100,000).
Men tend to fall from greater heights (ladders, home repairs) and carry heavier comorbidities, making recovery harder.
Age as a Mortality Multiplier
Fall-related mortality explodes with age:
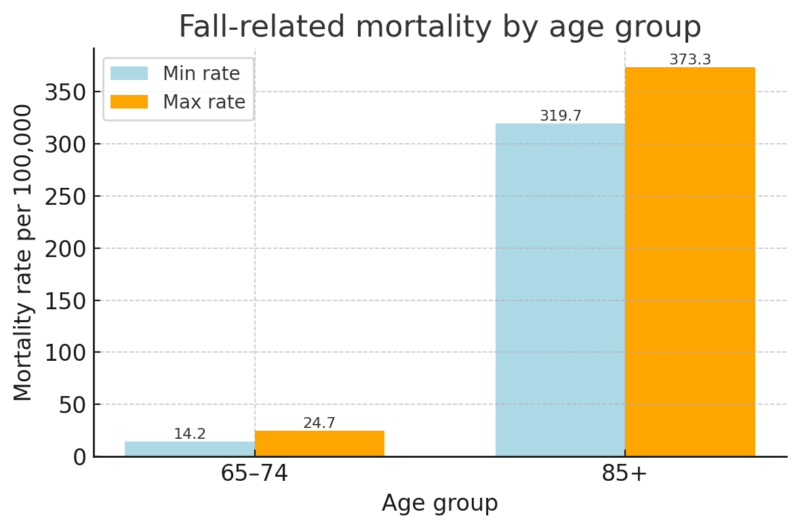
A fall after age 85 is often functionally equivalent to a terminal event; physiological reserve simply cannot withstand the trauma.
Geographic Variation
2023 state mortality rates ranged dramatically:
State
Fall Death Rate
Notes
Alabama
29.5
Lowest
Wisconsin
158.4
Highest
National Average
69.9
Baseline
Northern states with icy winters and rural regions without rapid trauma access show significantly higher fatality rates.
Why a “Simple Fall” Is Biologically Devastating

Ground-Level Falls: Low Energy, High Lethality
Most fatal falls in the elderly are ground-level falls (GLF), from a standing position. Yet older adults are three times more likely to die from a GLF than younger adults.
This reframes the fall: a short drop, but a massive physiological blow.
Frailty, Sarcopenia, and Osteoporosis
Frailty creates the perfect storm:
- Sarcopenia erodes shock-absorbing muscle tissue.
- Osteoporosis reduces the structural integrity of bone.
- Impaired homeostasis (cardiac, immune, metabolic) weakens trauma response.
A “minor” fall can shatter the femur or compress the spine because the bones simply cannot withstand the impact.
Cognitive and Sensory Decline
Balance is a sensory-motor reflex loop. In older adults:
- Vision loss doubles fall risk.
- Hearing loss triples it.
- Medications (sedatives, antidepressants, antihypertensives) impair reaction speed.
This combination makes falls more likely and more deadly.
Hip Fracture: The Injury That Redefines the Rest of Life
A hip fracture in an older adult is not just an orthopedic problem. In geriatric medicine, it is treated as a sentinel event: the moment when underlying frailty, chronic disease, and loss of physiological reserve become impossible to ignore.
From the day of the fracture, both survival odds and functional independence change sharply, often permanently.
One-Year and Five-Year Mortality: How Fast the Curve Drops
Hemiarthroplasty (partial hip replacement) is a standard surgical treatment for many geriatric hip fractures. Even with surgery and modern care, the survival curve is steeply downward.
Survival and Mortality After Hemiarthroplasty for Hip Fracture
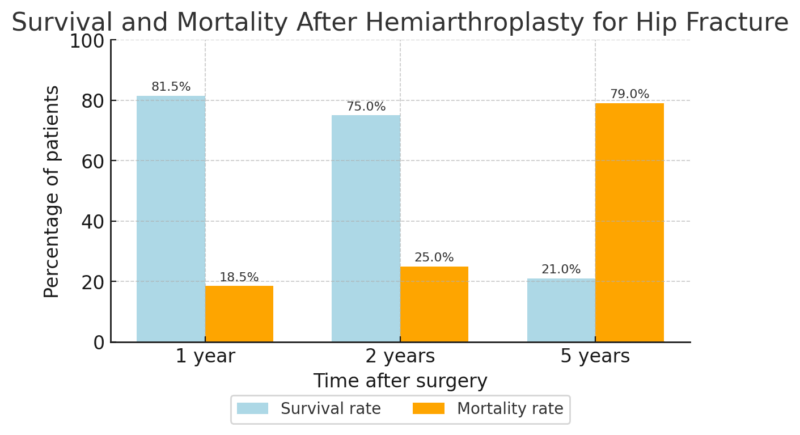
The key point is the five-year mark: nearly 5 in 10 patients have died within five years of a hip fracture, as per NCBI. That level of mortality is comparable to many aggressive malignancies.
Clinically, this is why a hip fracture is seen less as an isolated injury and more as a clear marker that the patient has entered a high-risk phase of life.
Who Dies Sooner: High-Risk Subgroups
- Patients over 80 years old
- Patients with dementia
- Nursing home residents
These groups illustrate that the fracture is not acting alone; it interacts with pre-existing vulnerability to accelerate decline.
Functional Decline: When Survival Does Not Mean Recovery
Even when older adults survive a hip fracture, most do not return to the life they had before. The injury often marks the transition from independent aging to dependency.
Key functional outcomes include:
- Less than 50% regain their pre-fracture independence
- Around 20% move permanently into long-term care
- Only about 40% of previously active seniors recover stair-climbing ability
You can think of this as a form of “social death”: the person may be alive, but their autonomy, mobility, roles, and identity are fundamentally altered.
After a hip fracture, the question is not only “How long will this person live?” but also “What kind of life will they be able to live from now on?”
Traumatic Brain Injury: The Silent Fatality of Falls

The Aging Brain Is Uniquely Fragile
Brain atrophy stretches the bridging veins. Even without striking the head, sudden acceleration can cause a subdural hematoma.
Falls cause:
- 61% of all severe TBIs in adults 65+.
Mortality Profile
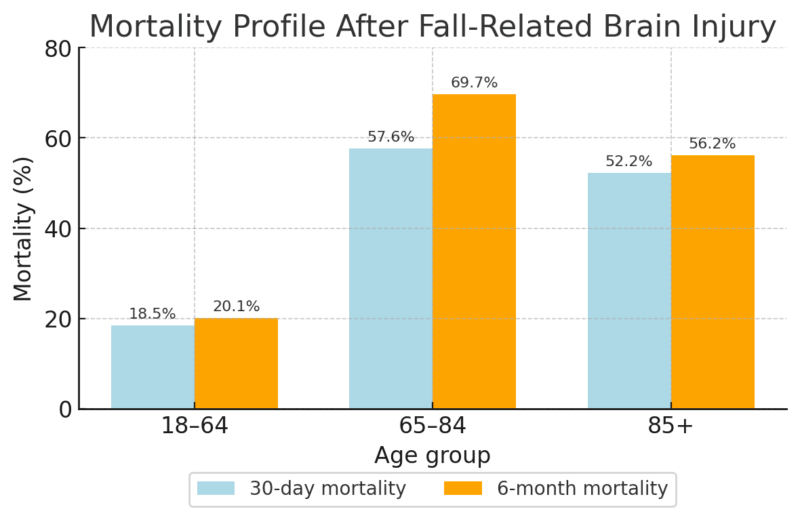
Chronic subdural hematoma alone carries a 32.9% one-year mortality according to Research Gate.
Functional Outcomes Are Bleak
Only 12% of older adults regain independent function after severe TBI. Most remain dependent or institutionalized.
Vertebral Compression Fractures: The Quiet Killer
Often dismissed as “minor,” vertebral compression fractures (VCFs) dramatically alter life expectancy.
Survival Statistics
- 8-fold increase in age-adjusted mortality.
- 1-year survival: 87%
- 5-year survival: 59%
- Overall 4-year mortality: 36%
Why VCFs Are Deadly
Pain and deformity reduce lung expansion. Patients develop:
- Atelectasis
- Fluid buildup
- Pneumonia (the leading cause of death in VCF patients)
Around 22% of VCF deaths are pneumonia-related.
The Chain Reaction: How a Fall Kills Slowly

The “Long Lie”
If someone falls and cannot get up:
- Rhabdomyolysis damages the kidneys
- Hypothermia accelerates organ failure
- Dehydration worsens shock
Long-lie victims have extremely high 6-month mortality.
Immobility → Clots → Pulmonary Embolism
Deep vein thrombosis is common after fractures. Pulmonary embolism often presents subtly and kills quickly.
Infection and Sepsis
- Bedsores
- Catheter-associated infections
- Pneumonia
- Sepsis mortality >25%
The Psychological Spiral: Fear of Falling as a Mortality Factor
@nikki.demus The “Fear of Falling” is a psychological factor that INCREASES fall risk. Once an older adult has a fall, especially if it’s a traumatic fall that results in injury, it can cause them to have a trauma response by not participating in daily activities like getting out of bed, walking, getting dressed, and going out into the community. The crazy thing is, lack of movement translates to loss of balance, strength and confidence, which moves towards the cycle of another fall . Follow me for more fall prevention tips and education 📚 @nikki.demus #fallprevention #occupationaltherapy ♬ original sound – nikki.demus
Fear of falling is one of the least visible yet most lethal consequences of a fall in older adults. It is not simply an emotional reaction; it is a measurable predictor of mortality.
Research shows that seniors who report intense fear have a Hazard Ratio of 1.86, meaning their risk of death is nearly double that of peers without fear, even after adjusting for physical health.
About 15% of older adults experience what researchers classify as “serious fear of falling,” and this fear often triggers a destructive behavioral cycle. In an attempt to stay safe, seniors restrict their movements: they stop going for walks, avoid errands, and limit physical activity.
This self-imposed inactivity rapidly accelerates muscle loss, weakens balance, and increases joint stiffness.
As the body deconditions, the likelihood of another fall rises sharply. At the same time, the emotional effects, social withdrawal, isolation, and depression further erode both physical resilience and overall health.
The result is a downward spiral where fear itself becomes a driving force of physical fragility, recurrent falls, and ultimately higher mortality.
Recovery and Rehabilitation: The Hard Truth
Recovery after a major fall is far more limited than most families expect.
Only about 30% of hip fracture survivors ever regain their previous level of daily functioning, and roughly one in five never return home, transitioning permanently into long-term care.
For seniors who suffer a traumatic brain injury, outcomes are slightly more varied; around two-thirds eventually return to community living, but a critical 10% remain permanently dependent, unable to resume independent life.
These numbers illustrate how a single fall can permanently reshape the trajectory of aging, often marking the point where independence gives way to long-term disability.
Prevention: The Only Proven Lifespan Extender

Because post-fall outcomes are so poor, prevention remains the only effective strategy for extending both lifespan and independence.
Strong evidence shows that exercise focusing on balance and leg strength, including Tai Chi and progressive resistance training, is the most powerful protection against falls.
Additional interventions such as medication reviews (especially reducing sedatives), vision correction like cataract surgery, targeted vitamin D and calcium supplementation, and simple home modifications (grab bars, proper lighting, non-slip surfaces) all work together to reduce risk.
Crucially, once a person has experienced a first fall, they enter a vulnerable period where a second fall dramatically increases mortality. Intervening during this window, through therapy, home adjustments, and medical optimization, can break the cycle before it becomes fatal.
Conclusion
A fall in later life exposes declining physiological reserve and often signals the beginning of accelerated health deterioration.
Serious injuries like hip fractures, TBIs, and vertebral compression fractures sharply shorten life expectancy, while fear-driven inactivity and immobility magnify the damage even without visible injuries.
The pattern is consistent: survival decreases, independence fades, and long-term outcomes worsen quickly. Yet the same data also shows that prevention, strengthening the body, improving balance, reducing environmental hazards, and correcting modifiable risks, remains the most powerful way to change this trajectory.
Prevention is not just helpful; it is the only reliable defense against the deadly cascade that a fall can unleash.