Weight loss drugs like Ozempic have become almost unavoidable over the past two years. I see them discussed everywhere, from doctors’ offices to casual conversations with friends.
They are often presented as a breakthrough solution. But new research presented in late 2025 suggests that when it comes to actual, sustained weight loss in real-world patients, surgery still outperforms these medications by a wide margin.
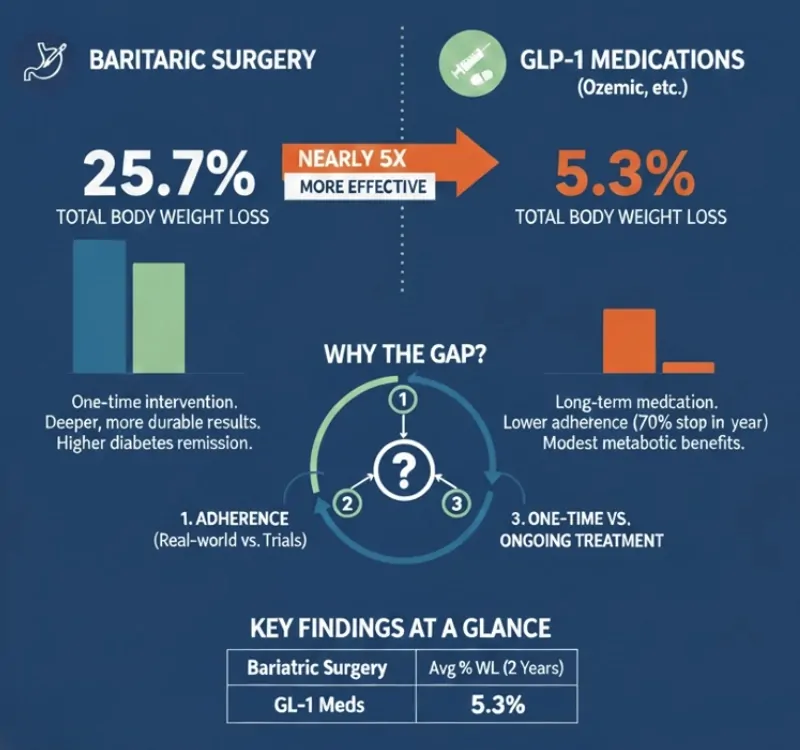
A study led by researchers at New York University found that bariatric surgery resulted in nearly five times more total weight loss than popular GLP-1 medications such as semaglutide (Ozempic) and tirzepatide over two years. The difference was not subtle. It was dramatic.
Table of Contents
ToggleHow the Study Compared Surgery and Ozempic
The NYU research team analyzed health records from patients who either underwent bariatric surgery or were prescribed GLP-1 weight loss drugs. Specifically, they looked at two well-established surgical procedures: sleeve gastrectomy and gastric bypass.
On the medication side, they focused on semaglutide and tirzepatide, both of which mimic the hormone GLP-1, which plays a key role in appetite regulation and blood sugar control.
To make the comparison fair, patients were carefully matched based on age, body mass index, and baseline blood sugar levels. This matching is important because it reduces the chance that one group simply started healthier or more motivated than the other.
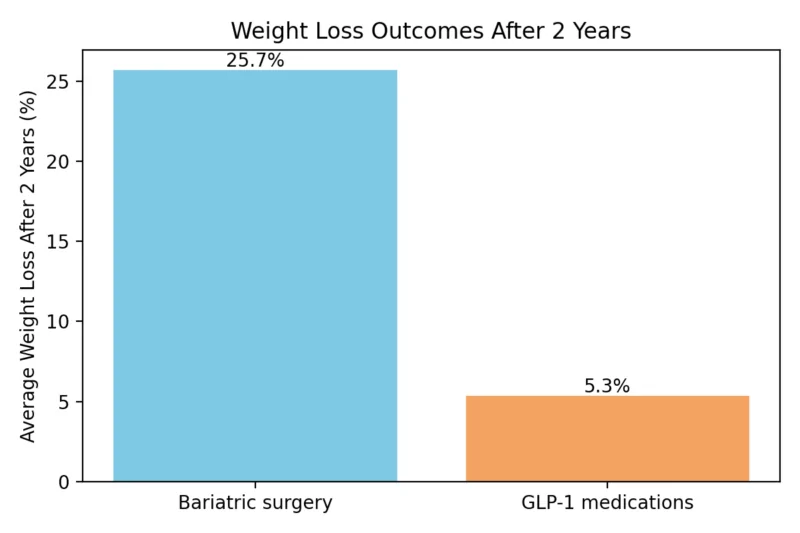
What the researchers found was striking. After two years, patients who had surgery lost an average of 25.7 percent of their total body weight. Those taking GLP-1 medications lost just 5.3 percent on average.
Why Real-World Results Look So Different From Clinical Trials
If you follow headlines closely, that 5.3 percent figure might surprise you. Clinical trials for GLP-1 drugs often report weight loss in the range of 15 to 21 percent. The NYU researchers addressed this gap directly.
According to Avery Brown, a surgical resident at NYU who presented the findings earlier in 2025, clinical trials do not always reflect how people use medications in everyday life.
In controlled studies, patients receive close monitoring, frequent follow-ups, and strong incentives to stay on treatment. In the real world, adherence drops quickly.
Data cited by the researchers suggest that up to 70 percent of patients stop taking GLP-1 medications within one year. Cost, side effects, supply issues, and simple fatigue with long-term injections all play a role.
Surgery, by contrast, is a one-time intervention. While it requires lifelong lifestyle adjustments, it does not rely on ongoing medication compliance.
Even over shorter time frames, surgery consistently produced greater weight loss than drugs, reinforcing the idea that the difference is not just about long-term drop-off in medication use.
Weight Loss Outcomes at a Glance
Diabetes Control and Metabolic Health
Weight loss was not the only outcome the researchers examined. Both GLP-1 drugs and bariatric surgery are known to improve blood sugar control, which is why semaglutide was originally approved as a treatment for type 2 diabetes.
In this study, bariatric surgery was associated with even greater improvements in blood sugar regulation compared to medication alone. That finding aligns with decades of data showing that metabolic surgery can lead to diabetes remission in some patients, not just improvement.
This does not mean GLP-1 drugs lack metabolic benefits. Multiple studies have linked semaglutide to reduced cardiovascular risk and even lower rates of certain cancers.
The key point is that, when measured side by side, surgery delivered bigger and more durable metabolic changes.
Important Context and Potential Bias
It is worth noting that the study was funded by the American Society for Metabolic and Bariatric Surgery (ASMBS). That does not invalidate the findings, but it does mean they should be interpreted carefully. Independent replication will be important.
ASMBS President Ann M. Rogers, who was not directly involved in the research, summarized the takeaway clearly: while both treatments help patients lose weight, surgery remains the most effective and long-lasting option currently available.
Why Surgery Is Still Rare Despite Strong Results
Despite its effectiveness, bariatric surgery remains underused. Only a small fraction of people who medically qualify for surgery ever choose it. Fear of invasive procedures, misconceptions about safety, limited access, and insurance barriers all contribute.
GLP-1 drugs, on the other hand, have seen explosive growth. Prescriptions doubled between 2022 and 2023, driven by aggressive demand and widespread media coverage. For many patients, the idea of an injection feels less intimidating than surgery, even if the results are more modest.
But surgery is not an easy path. These procedures are permanent, require strict dietary adherence, and come with real risks. They are not a shortcut, and they do not eliminate the need for lifestyle changes.
What This Means for Patients in 2025
The study does not argue that Ozempic or similar drugs should be abandoned. Instead, it highlights a growing gap between expectations and reality. Many people assume GLP-1 drugs will deliver dramatic, lasting weight loss on their own.
For most patients, that has not proven true outside clinical trials.
Future research, according to NYU bariatric surgeon Karan Chhabra, will focus on identifying which patients are best suited for medication, which benefit most from surgery, and how factors like out-of-pocket costs affect long-term success.
The research was presented at the ASMBS Annual Meeting in 2025, and it builds on earlier findings published in mid-2025.
The Bottom Line
@kukrejamd People always want to know, which is better. Well, the first study comparing modern drugs to surgeries that we’ve been doing for decades is out, and as you guessed it, bariatric surgery win. #bariatricsurgery #weightloss #glp1 #medication ##sleevegastrectomy #gastricbypass #medicine #surgery #healthcare ♬ original sound – Sachin Kukreja MD • Bariatrics
In real-world use, bariatric surgery produces far greater and more durable weight loss than Ozempic and similar GLP-1 drugs.
Medications still play an important role, especially for patients unwilling or unable to undergo surgery, but the data suggest expectations should be recalibrated.
Weight loss remains complex, personal, and heavily influenced by long-term adherence, not just medical innovation.
Related Posts:
- Ozempic-Style Weight Loss Drugs for Cats Are Now…
- Weight Loss Without Injections? Wegovy’s New Pill Is…
- New Research Shows How the Brain Adapts Faster Than AI
- Adult Daily Protein Intake Much More Than Recommended
- Wyoming Fatal Crashes in 2025 (So Far) vs. Previous…
- Anxiety and Depression Statistics - CBT Effective…