If you look at cancer in the United States over the past quarter-century, the story is one of declining death rates but shifting risks by age and cancer type.
According to the American Cancer Society (2025), overall cancer mortality has fallen by about 34% from its 1991 peak, which translates into roughly 4.5 million fewer deaths. Between 2013 and 2022 alone, the national cancer death rate declined by an average of 1.7% per year in men and 1.3% in women.
Yet incidence tells a different story. Data from the National Cancer Institute’s SEER program shows that overall incidence flattened, with men experiencing declines that later leveled off, while women’s incidence rose slightly every year since 2003 (except 2020, when pandemic disruptions delayed diagnoses).
Meanwhile, cancers in younger adults (especially colorectal cancer in people under 55) have become more common and more deadly, signaling a generational shift.
Americans are less likely to die of cancer than 25 years ago, but younger adults are facing new risks, and certain cancer types like prostate, pancreas, and colorectal remain stubborn challenges.
Table of Contents
ToggleLong-Term National Trends
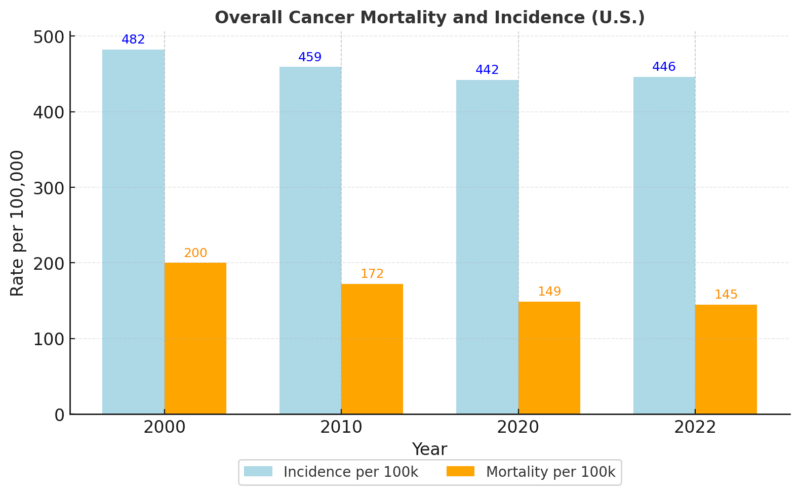
Overall Mortality and Incidence
According to SEER and CDC Vital Statistics, the age-adjusted cancer death rate dropped from ~215 per 100,000 in 1991 to ~145 per 100,000 by 2022.
At the same time, incidence stayed near 440 to 450 per 100,000, showing that prevention and treatment, not fewer diagnoses, drove mortality gains.
Trends by Cancer Site
Lung Cancer
Lung cancer tells the clearest success story. According to the CDC, death rates fell more steeply than for any other cancer, driven by reduced smoking, better screening, and new immunotherapies.
In 2018 to 2022, lung incidence averaged 47.8 per 100k, with deaths at 31.5 per 100k, a sharp decline from early-2000s levels.
Colorectal Cancer
Colorectal incidence overall has declined in older adults thanks to colonoscopy screening, but rates in younger adults (<55) have been rising ~1% per year since 2000.
According to the ACS, colorectal cancer is now the second-leading cause of cancer death in men under 50.
Prostate Cancer
After a sharp decline in diagnoses following changes in PSA screening guidelines in the early 2010s, incidence has climbed again, up about 3% per year since 2014.
More concerning is the increase in regional and distant-stage prostate cancers, which are harder to treat effectively.
Melanoma
Melanoma deaths fell significantly between 2013 and 2022, reflecting the impact of checkpoint inhibitor immunotherapies. The death rate dropped to about 2.0 per 100k by 2023, down from much higher levels in the early 2000s.
Pancreatic Cancer
Unlike most major cancers, pancreatic incidence and deaths have continued to rise slowly but steadily, now at 13.8 incidence and 11.3 deaths per 100k. This persistence makes it one of the deadliest cancers, largely because most cases are diagnosed late.
Cervical Cancer
Screening and HPV vaccination have sharply reduced cervical precancers in younger women, yet incidence among women aged 30 to 44 is increasing by about 1.7% per year.
According to the National Cancer Institute, this reflects gaps in screening uptake and follow-up care.
Cancer in Younger Adults: An Alarming Shift
One of the most striking and worrying shifts in the U.S. cancer landscape over the last 25 years has been the rising burden among adults under 55 years of age. While overall cancer mortality has declined in the population at large, younger cohorts are seeing the opposite trend: incidence and deaths are climbing modestly but steadily.
According to the National Cancer Institute’s SEER data, cancers such as colorectal, kidney, pancreas, and uterine are among those showing the strongest increases in this group. The American Cancer Society reported in 2024 that cancer deaths in people under 55 are rising by about 1% per year, a reversal of the progress seen in older age groups.
This trend matters because cancer in younger adults carries different consequences. Many are in their prime working years, raising families, or still building financial security. A cancer diagnosis at this age brings a higher economic burden, long-term survivorship challenges, and greater psychosocial impact compared to older adults.
Which Cancers Are Rising in Younger Adults?
- Colorectal cancer: Perhaps the most publicized shift. According to ACS, incidence in adults under 50 has risen by nearly 2% annually since the mid-1990s, and it is now the second leading cause of cancer death in men under 50. Screening guidelines have been lowered to age 45 in response.
- Kidney cancer: Incidence has been rising slowly in younger adults, with obesity and hypertension strongly linked as risk factors.
- Pancreatic cancer: Once almost exclusively a disease of older age, pancreatic cancer rates are creeping upward in adults under 55. Though rare in absolute terms, its lethality makes the trend concerning.
- Uterine (endometrial) cancer: Rising steadily in women under 50, linked to obesity and metabolic health, with disproportionate impacts on Black women.
Possible Drivers of The Trend
Researchers point to several overlapping explanations:
- Lifestyle changes: Rising rates of obesity, diabetes, and sedentary habits in younger generations are strongly tied to colorectal, kidney, and uterine cancers.
- Dietary patterns: Increased consumption of ultra-processed foods, sugary drinks, and low fiber intake are implicated, especially in early-onset colorectal cancer.
- Environmental exposures: Chemicals, endocrine disruptors, and pollutants may be playing a role, though evidence is still emerging.
- Microbiome shifts: Early antibiotic exposure, processed diets, and gut microbiome alterations are being studied as contributors to digestive cancers.
- Delayed or reduced screening: Many cancers in younger adults are diagnosed at later stages because routine screening traditionally began later in life.
Cancers Rising in Adults Under 55 (U.S., 2000–2025)
Cancer Type
Trend (Incidence/Deaths)
Key Stats in Younger Adults
Likely Drivers
Colorectal
↑ ~2% annually under 50
Now the 2nd leading cause of cancer death in men <50
Obesity, diet, microbiome, reduced activity
Kidney
Gradual rise
Steady increase in the <55 group, more in men
Obesity, hypertension, diabetes
Pancreatic
Slow but consistent ↑
Rare but more common than 25 years ago; high fatality
Obesity, smoking, diabetes, and late detection
Uterine (Endometrial)
↑ in women under 50
Rising sharply, disproportionate in Black women
Obesity, metabolic health, and hormones
Breast (subtype: ER-)
Stable overall, but ↑ in aggressive forms
Triple-negative breast cancer disproportionately affects younger women
Genetic factors, obesity, and unknown environmental causes
Why This Matters for The Next 25 Years

The rise of cancer in younger Americans is a generational warning sign. While progress has been made in reducing overall cancer deaths, these shifts suggest that prevention strategies must adapt.
Screening guidelines have already been adjusted (colorectal screening now begins at 45 instead of 50), but more work is needed in obesity prevention, early symptom awareness, and research into environmental exposures.
In effect, cancer is no longer just a disease of aging. The medical community is being forced to rethink its approach, as younger patients increasingly enter oncology wards with cancers once considered “diseases of older age.”
Disparities by Race, Sex, and Region
Even as national cancer mortality has dropped steadily over the last 25 years, the benefits have not been evenly shared across racial groups, sexes, and geographic regions.
The data highlight how social, economic, and healthcare access factors continue to shape who gets cancer, when it’s detected, and how likely patients are to survive.
Racial and Ethnic Disparities
Prostate cancer is perhaps the most well-documented example. According to SEER and CDC data, Black men have incidence rates about 70% higher than White men and mortality rates more than double.
This pattern has persisted for decades despite overall improvements in detection and treatment. Researchers point to a mix of factors: genetics and tumor biology may play a role, but access to early detection and quality treatment are equally critical. Other disparities are also notable:
- Breast cancer mortality in Black women remains ~40% higher than in White women, even though incidence is similar. Later-stage diagnoses and lower access to advanced therapies explain much of this gap.
- Liver and stomach cancers are more common in Asian and Hispanic populations, tied to viral hepatitis prevalence, Helicobacter pylori infections, and environmental exposures.
- Cervical cancer continues to disproportionately affect Hispanic and Black women, reflecting gaps in screening and vaccination uptake. In many underserved clinics, routine testing equipment, such as a hematology analyzer for the lab, is not always available, which limits early detection and monitoring for related conditions that influence cancer outcomes.
Geographic Disparities

Cancer risk and outcomes vary widely by where people live. Southern states consistently report higher lung and cervical cancer incidence and mortality.
According to the American Cancer Society, these patterns are strongly linked to higher smoking prevalence, lower HPV vaccination rates, and reduced access to screening programs.
In contrast, states like Massachusetts, with robust public health infrastructure, show significantly lower mortality rates across multiple cancer types.
Rural versus urban divides are also significant. Rural Americans face higher death rates from preventable cancers due to fewer cancer centers, longer travel distances for treatment, and higher rates of poverty and uninsured populations.
Sex Differences
Cancer incidence trends also differ by sex. Over the past two decades, men’s overall incidence fell, then flattened, while women’s incidence has slowly risen.
Much of this rise in women is due to breast cancer, thyroid cancer, and certain gastrointestinal cancers, some of which are tied to obesity and hormonal factors.
Mortality, however, continues to decline in both sexes, though men still experience a higher overall cancer death rate.
Key Cancer Disparities in the U.S. (2000–2025)
Group
Cancer Type
Disparity
Likely Drivers
Black men
Prostate
70% higher incidence; >2× mortality vs White men
Genetics, late diagnosis, unequal access to care
Black women
Breast
~40% higher mortality despite similar incidence
Later detection, treatment gaps, tumor biology
Hispanic and Black women
Cervical
Higher incidence and death rates
Lower Pap test rates, HPV vaccination gaps
Asian and Hispanic populations
Liver, stomach
Higher incidence
Hepatitis B/C, H. pylori, dietary/environmental factors
Southern states
Lung, cervical
Higher rates
Smoking prevalence, screening gaps, and limited public health funding
Women overall
Breast, thyroid, GI
Rising incidence
Obesity, hormones, detection patterns
Rural Americans
Preventable cancers (lung, cervical, colorectal)
Higher mortality
Limited healthcare access, economic barriers
What Drives These Trends?
- Prevention: Tobacco control policies and HPV vaccination are major success stories.
- Screening: Colonoscopy, Pap tests, mammography, and low-dose CT scans for lung cancer have all changed detection patterns.
- Treatment advances: Targeted therapies and immunotherapies have redefined survival in cancers like melanoma and lung cancer.
- COVID-19 pandemic effects: In 2020, screening interruptions temporarily lowered recorded incidence, though many of those “missing” cancers showed up in later years.
Snapshot of Current Rates (2018 to 2022, SEER Data)
| Cancer Type | Incidence (per 100k) | Mortality (per 100k) | 25-Year Trend |
| All sites | 446 | 145 | Mortality ↓ 34%, incidence flat |
| Lung | 47.8 | 31.5 | Sharp declines in deaths |
| Colorectal | ~36 | ~13 | Deaths ↓ in older adults, ↑ in <55 |
| Prostate | 113 | ~18 | Incidence has been rising since 2014 |
| Pancreas | 13.8 | 11.3 | Slow rise in both |
| Melanoma | 22 | 2.0 | Deaths fell rapidly post-2013 |
| Cervical | 7.7 | 2.2 | Overall decline, but ↑ in 30–44 |
Methodology
This article was crafted using the most recent publicly available data from the American Cancer Society (ACS), the National Cancer Institute’s SEER program (Surveillance, Epidemiology, and End Results), and CDC Vital Statistics. We focused on 25-year trends (2000–2025) to capture long-term shifts in both incidence and mortality.
- Data sources: ACS Cancer Facts & Figures 2024/2025, SEER incidence and mortality tables (2018 to 2022 most recent complete set), and CDC provisional death statistics.
- Measures: All cancer rates are age-adjusted per 100,000 population to allow comparison across time and demographics.
- Trend analysis: Annual percent changes were taken from ACS and SEER publications, with special emphasis on key cancer sites (lung, colorectal, prostate, pancreas, melanoma, and cervical).
- Disparities: Racial, sex-based, and regional disparities were highlighted using comparative statistics published by ACS and SEER, supplemented by CDC geographic mortality data.
- Limitations: 2020 data show a lower recorded incidence due to COVID-19 disruptions in screening and diagnoses. This was noted in the interpretation.
By combining authoritative datasets with contextual analysis, the article aims to provide readers with both a statistical snapshot and a narrative understanding of how cancer in the U.S. has evolved over the past 25 years.
Endnote
@sagesteeleshow “The highest cancer rates in human history… right here in America.” Calley Means — senior adviser to Secretary of Health and Human Services Robert F. Kennedy Jr. — reveals a shocking truth: out of 212 countries, the U.S. leads the world in cancer rates, and Iowa now holds the highest rate ever recorded in human civilization. Yet instead of focusing on prevention, America spends 40x more on cancer treatments than on finding the root causes. $400 billion a year… and cancer rates keep rising. The question is: what’s in our environment that’s fueling this crisis? Full episode now on YouTube. #iowa #cancer #cancertreatment ♬ original sound – Sagesteeleshow
Over the past 25 years, the U.S. has made historic progress against cancer deaths, cutting mortality by more than a third. Advances in prevention, early detection, and treatment are saving lives every year.
At the same time, new challenges are emerging, particularly the rise of colorectal and other cancers in younger adults, the persistence of pancreatic cancer, and disparities across race and geography.
The takeaway is clear: while Americans are less likely to die of cancer today than in 2000, the fight is not finished. Continued investment in screening access, public health prevention, and breakthrough therapies will determine whether the next 25 years see equally dramatic gains.
Related Posts:
- Average Home Value Increase Per Year in the US, 5…
- How Have U.S. Birth Rates Changed Over the Last 20 Years?
- How Washington DC’s Population Has Evolved Over the…
- Stomach Cancer - Survival Rates and the Importance…
- Statistics on Statin Use in The US - The Impact of…
- Wyoming Fatal Crashes in 2025 (So Far) vs. Previous…