The National Health and Nutrition Examination Survey (NHANES) is a groundbreaking program that has revolutionized our understanding of health and nutrition in the United States.
It is a division of the Centers for Disease Control and Prevention (CDC), NHANES provides unparalleled insights into the health, nutritional status, and well-being of the U.S. population.
For over six decades, NHANES has collected comprehensive data that have shaped medical practices, public health policies, and nutrition guidelines.
Table of Contents
ToggleThe Origins of NHANES
NHANES traces its roots to the National Health Survey Act of 1956, which authorized the systematic collection of data on the health of Americans. Initially focused on health examinations, the program expanded in the 1970s to include nutritional assessments, marking the birth of NHANES as we know it today.
Key milestones in the evolution of NHANES:
- 1960-1962: The first National Health Examination Survey targeted adults aged 18-74 to collect data on general health indicators.
- 1971-1974: NHANES I incorporated nutrition as a focus area, assessing dietary intake, biochemical markers, and physical measurements.
- 1976-1980: NHANES II extended its scope to include children as young as six months and seniors up to 74 years old.
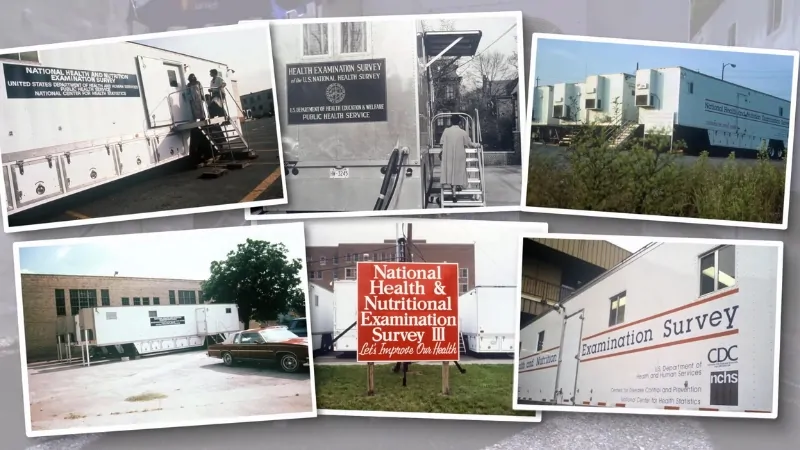
- 1988-1994: NHANES III introduced mobile examination centers (MECs), enhancing accessibility and efficiency in data collection.
- 1999-Present: NHANES became a continuous survey, allowing for real-time tracking of health trends and more responsive public health initiatives.
Purpose and Objectives
According to CDC NHANES is designed to:
- Assess Health and Nutrition: Evaluate the prevalence of diseases, risk factors, and dietary habits among diverse population groups.
- Track Trends Over Time: Monitor changes in health and nutrition indicators to understand evolving public health challenges.
- Support Policy and Research: Provide data that inform clinical guidelines, public health interventions, and government policies.
How NHANES Works

Sampling and Participants
NHANES uses a stratified, multistage probability sampling design to ensure that its findings represent the entire U.S. population, including underrepresented groups.
Each year, approximately 5,000 individuals are selected from across the country.
Oversampling of high-risk groups, such as children, seniors, and low-income households, improves the reliability of data for these populations.
Data Collection Components
NHANES collects a wide range of data through:
- Interviews: Conducted in participants’ homes, covering topics such as:
- Health history and medical conditions.
- Dietary habits and supplement use.
- Socioeconomic and demographic factors.
- Examinations: Performed in state-of-the-art mobile examination centers (MECs), including:
- Physical measurements (e.g., height, weight, body composition).
- Dental exams and vision tests.
- Laboratory tests using blood and urine samples.
- Special Tests and Procedures: Depending on age and health status, participants may undergo:
- Bone density scans.
- Skin allergy tests.
- X-rays of the chest and spine.
Mobile Examination Centers (MECs)
CDC in 1999 noted that one of NHANES’s most innovative features is its use of mobile examination centers—custom-designed facilities that travel to survey locations nationwide. MECs ensure that data collection is:
- Standardized: All procedures are performed under controlled conditions by highly trained medical staff.
- Accessible: MECs reduce barriers to participation by bringing the survey to communities.
Key Achievements and Impact
Over the years, NHANES has contributed significantly to public health advancements:
1. Diagnosing Undiagnosed Conditions
NHANES data revealed that a significant percentage of adults with hypertension and diabetes were unaware of their conditions. These findings prompted widespread screening and early intervention programs.
2. Developing Growth Charts
NHANES measurements were used to create the pediatric growth charts that doctors rely on to track children’s growth and development. These charts are now a global standard.
3. Reducing Lead Exposure
In the 1970s, NHANES provided the first concrete evidence that Americans had dangerously high levels of lead in their blood, primarily due to leaded gasoline and paint. These findings led to federal regulations that virtually eliminated lead exposure, reducing blood lead levels in the population by over 90%.
4. Improving Nutrition
NHANES data highlighted widespread nutrient deficiencies, such as low iron and folate levels. In response, the government mandated the fortification of foods, such as adding iron to cereals and folic acid to grain products, to combat these deficiencies.
Data Access and Usage
NHANES data is a valuable resource for researchers, policymakers, and healthcare providers.
Public-Use Data
Freely available on the NHANES website, public-use datasets are anonymized to protect participants’ privacy. These datasets have been used in countless studies to analyze health trends and disparities.
Restricted-Use Data
For more detailed analyses, researchers can request access to restricted-use data through the NCHS Research Data Center (RDC). These datasets include sensitive information, such as geographic identifiers and finer demographic details.
Research Applications
NHANES data has been instrumental in:
- Tracking obesity trends.
- Monitoring the effects of environmental exposures.
- Evaluating the effectiveness of public health interventions.
Quality Assurance

NHANES maintains rigorous quality control measures at every stage of data collection and processing:
- Interviewers undergo extensive training in survey protocols.
- Data is routinely reviewed for accuracy and consistency.
- Laboratory tests follow strict protocols to ensure reliability.
Recent and Ongoing Initiatives
NHANES continues to adapt to meet the nation’s evolving health needs:
- Continuous Updates: New health topics and diagnostic tests are regularly incorporated.
- COVID-19 Response: NHANES added questions and procedures to capture data on the pandemic’s impact on health and nutrition.
- Health Disparities: Oversampling and targeted studies address the needs of underserved populations.
Challenges and Opportunities

Challenges
- Recruitment and Participation: Maintaining high response rates is crucial for data accuracy.
- Funding Limitations: Budget constraints can restrict the scope of the survey.
- Privacy Concerns: Balancing data accessibility with participant confidentiality remains a priority.
Opportunities
- Technological Advancements: Digital tools and telehealth could expand data collection capabilities.
- Longitudinal Studies: Follow-up surveys could provide deeper insights into long-term health trends.
Conclusion
The National Health and Nutrition Examination Survey (NHANES) is more than a survey; it is a cornerstone of public health research and policy. By collecting comprehensive and reliable health data, NHANES has transformed our understanding of nutrition, chronic diseases, and environmental exposures.
Its findings continue to guide efforts to improve health outcomes and reduce disparities across the United States.
As NHANES moves forward, it remains a vital resource for addressing today’s health challenges and preparing for the public health needs of tomorrow.
References
- NCBI Bookshelf – The National Health Survey Act and Health Data Collection
- CDC NHANES I – NHANES I Overview
- CDC NHANES II – NHANES II Overview
- CDC NHANES III – NHANES III Data Files
- CDC NHANES About – About NHANES
- CDC NHANES MEC Manual (1999) – NHANES Mobile Examination Centers (MECs)
- PubMed Central (PMC) – NHANES COVID-19 Response
Related Posts:
- Can the Brain Truly Recover from Addiction? Here’s…
- Health Insurance Coverage - National Health…
- Health Statistics and the Rising Costs of Personal…
- States That Spend the Most (and Least) Per Resident…
- How Lighting Affects Mental Focus, Sleep, and Eye Health
- Mental Health Trends Among Veterans – PTSD and…