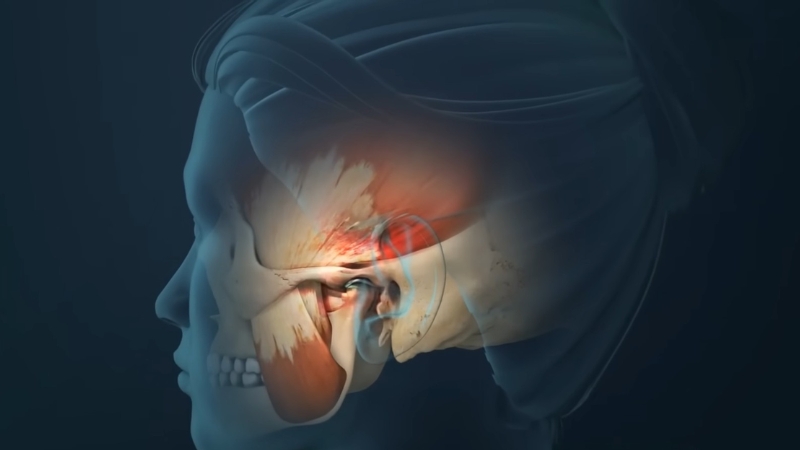
Temporomandibular disorders, commonly referred to as TMDs, include more than 30 conditions affecting the temporomandibular joints, masticatory muscles, and related structures.
These disorders influence jaw movement, joint function, and muscular coordination.
Pain, joint sounds, limited opening, locking, and functional impairment are common clinical features.
Impact on daily life can be substantial. Eating, speaking, facial expression, and even breathing may become difficult in moderate to severe cases.
Persistent symptoms can interfere with sleep, work performance, and social interaction.
Quality of life often declines when pain becomes chronic or fluctuates unpredictably.
Table of Contents
TogglePrevalence and Public Health Significance
Temporomandibular disorders represent a significant yet often underestimated public health concern.
Jaw disorders affect millions of people worldwide, affecting individuals across age groups, with higher prevalence reported in women and adults in early to middle adulthood.
Estimates vary by study and population, yet national data in the United States suggest that between 10 and 35 million individuals report TMJ-related symptoms, such as:
- Pain
- Clicking
- Restricted movement
Reported symptoms frequently include:
Many additional cases likely remain undiagnosed or untreated due to normalization of symptoms, lack of awareness, or limited access to specialized care.
Mild cases may progress over time when early intervention is absent.
Clinical care remains inconsistent across settings. Complementary approaches such as modern TMJ therapy, including infrared light therapy, are also being used to reduce pain and improve function in some patients.
Diagnostic criteria vary among providers, and treatment recommendations differ across dental, medical, and pain specialties.
Patients may receive contrasting opinions regarding occlusion, splint therapy, physical rehabilitation, pharmacologic management, or surgical intervention.
Lack of standardized pathways contributes to uneven outcomes and patient confusion.
Repeated consultations, trial-and-error treatment approaches, and inconsistent follow-up increase frustration and cost.
Historical Context of TMD Research and Care
Development of TMD research and clinical management has occurred across multiple disciplines, often without coordination.
Independent professional traditions shaped diagnostic philosophies and treatment priorities.
Key contributing fields include:
Fragmented approaches have produced mixed evidence and conflicting recommendations.
Some patients have undergone irreversible procedures without clear benefit, including extensive occlusal adjustments or surgical interventions.
Others received minimal intervention despite significant disability and psychosocial distress.
National calls for reform have stressed the need for coordinated, evidence-based, patient-centered models.
Greater integration across disciplines has been identified as essential to improve the reliability of diagnosis and the consistency of care delivery.
Emergence of the TMD IMPACT Initiative
View this post on Instagram
A post shared by University at Buffalo School of Dental Medicine (@ubdentalmedicine)
Growing recognition of fragmented research and clinical care led to the creation of a national collaborative effort.
TMD Collaborative for Improving Patient-Centered Translational Research, known as TMD IMPACT, represents a major effort supported by NIH and NIDCR.
The initiative aims to establish a national interdisciplinary research consortium focused on advancing basic science, clinical research, and practical application in TMD care.
Consortium framework supports coordinated infrastructure, shared protocols, and harmonized data collection.
Central objectives include:
Structured governance and sustained funding are intended to reduce duplication of effort and promote cumulative scientific progress.
State of the Evidence
Research in temporomandibular disorders has expanded in scope and methodological rigor over the past decade.
Increasing recognition of biological, psychological, and social contributors to jaw pain has reshaped scientific priorities.
Current evidence portrays TMD as a heterogeneous group of conditions requiring refined classification and coordinated investigation.
Pain Patterns and Clinical Subtypes

Accumulating data indicate that TMD cannot be adequately described as a single clinical entity.
Growing evidence suggests that TMD represents a spectrum of conditions with varying severity, symptom distribution, and functional impact.
Research published in 2022 identified distinct pain patterns among individuals with TMD, separating patients into high-impact and low-impact categories based on physical and psychological burden.
Patients categorized as having high-impact pain demonstrated greater symptom intensity and broader life disruption.
Short-term pain fluctuations occurred more frequently in this group and may function as a clinical marker of more severe disease.
Observed features in high-impact cases include:
Low-impact pain cases showed fewer fluctuations and less associated disability.
Stable symptom patterns were more common in these individuals, and functional impairment was typically limited.
Variability in daily pain intensity may therefore hold diagnostic and prognostic value, supporting early identification of patients at risk for chronic disability.
Psychosocial and Functional Complexity
Chronic TMD frequently involves central pain amplification and psychosocial influences.
Anxiety, depression, stress exposure, and sleep disturbance can change neural processing and pain perception.
Individuals with high-impact pain typically report more widespread physical symptoms and greater functional limitation across daily activities.
Clinical presentation often extends past localized jaw discomfort. Common patterns include:
Central sensitization mechanisms may amplify nociceptive signaling and sustain pain in the absence of clear structural pathology.
Psychological distress can further influence coping behaviors, treatment adherence, and recovery trajectory.
Musculoskeletal findings alone do not account for symptom severity in many patients.
Gaps in Evidence and Care Delivery

Despite scientific progress, significant gaps persist in the translation of research findings into routine practice.
Comprehensive reviews have concluded that care delivery remains fragmented and insufficiently guided by strong evidence-based protocols.
Clear, standardized clinical pathways are lacking in many health systems, resulting in variability in diagnostic labeling and intervention choice.
Educational training for dentists, physicians, and allied health professionals often provides limited exposure to chronic pain science and interdisciplinary management models.
Identified shortcomings include:
Consequences of these systemic gaps are observable in clinical outcomes.
Inconsistent diagnostic labeling, variable treatment sequencing, limited outcome tracking, and unequal access to comprehensive care continue to affect long-term prognosis.
Patients may cycle through multiple providers without cohesive coordination.
TMD IMPACT Initiative
Growing recognition of fragmented research efforts prompted the development of a coordinated national consortium.
TMD Collaborative for Improving Patient-Centered Translational Research, known as TMD IMPACT, represents a major effort supported by NIH and NIDCR.
Initiative seeks to strengthen collaboration and accelerate translation of scientific findings into improved care delivery.
Goals of TMD IMPACT

The consortium’s mission centers on advancing basic and clinical research with clear translational relevance.
Primary goals include the development of validated diagnostic methods and evidence-based treatments suitable for integration into routine practice.
Population-based research addressing disease burden, healthcare costs, and disparities forms another core objective.
Training programs aim to prepare investigators capable of bridging laboratory discoveries with clinical implementation.
Integrated approach seeks to align scientific progress with measurable improvements in patient-centered outcomes.
Funding and Consortium Development
Phased funding supports systematic growth of infrastructure.
Planning grants awarded in 2023 laid the groundwork for collaboration networks, shared databases, and governance structures.
Early awards totaled $2.8 million to support partnership building and research capacity expansion.
Cooperative agreement awards initiated in 2025 formalized consortium operations. Funding mechanisms promote multicenter clinical trials, harmonized data standards, and coordinated analytic strategies.
Structured oversight enhances accountability and consistency across participating institutions.
Multidisciplinary and Trans-NIH Integration
2/3 Do you suffer from a #TMD (temporomandibular disorder)? The pain can be intense, but there are ways to ease it at home. #PainAwarenessMonth #NIHPainProgress #TMJ https://t.co/pafIITvkmy pic.twitter.com/yTX9DH8rtT
— NIDCR at NIH (@NIDCR_NIH) September 20, 2024
Collaboration across NIH institutes promotes integration of pain science, tissue engineering, neuroscience, and population health research.
Cross-disciplinary participation strengthens study design and broadens investigative scope.
Coordinated governance structures facilitate:
Integrated framework reduces isolation of research silos and supports cumulative scientific advancement.
Patient-Centered Research Priorities
Active patient involvement shapes research direction and outcome measurement at each stage of project development.
Engagement of individuals living with TMD informs the selection of meaningful endpoints that capture multidimensional impact.
Domains commonly assessed include:
Patient partnership enhances ethical accountability and strengthens the relevance of research findings to real-world care.
Closing Thoughts

TMD IMPACT is positioned to promote evidence-based, multidisciplinary research and coordinated care frameworks that replace fragmented practices.
Advances in diagnostics, technology, and patient-centered methodology are expected to refine classification and tailor treatments more effectively.
Ongoing focus on translational science, workforce preparation, and integrated clinical pathways aims to improve outcomes for individuals living with temporomandibular disorders.







