Stress has always been a part of modern life, but in the United States, recent surveys suggest it is becoming a defining feature of daily living for millions of people.
According to the American Psychological Association’s (APA) “Stress in America” survey, a majority of Americans say their stress levels have increased over the past five years, with around 75% reporting physical or emotional symptoms related to stress.
This is not a small bump – it’s a sustained upward trend, fueled by a mix of economic uncertainty, political polarization, public health challenges, and personal financial strain.
Gallup’s Global Emotions Report (2023) found that about 49% of Americans experience significant daily stress, one of the highest rates among high-income nations. For context, that’s nearly one in every two adults walking through life with a daily undercurrent of tension.
The APA also points out that financial stress is consistently ranked as the top stressor, ahead of work, health concerns, and personal relationships.
Table of Contents
ToggleBreaking Down the Top Sources of Stress
Source of Stress
Percentage of Adults Reporting It as Significant
Notable Impacts
Personal Finances
~66% (APA, 2023)
Anxiety, sleep disruption, and delayed healthcare visits
Inflation & Cost of Living
~64% (APA, 2023)
Budget strain, reduced spending on essentials
Work-Related Stress
76% (American Institute of Stress)
Burnout, reduced productivity, and absenteeism
Health Concerns (Personal & Family)
61% (APA, 2023)
Worry, preventative care delays
Political Climate & News
55% (APA, 2023)
Emotional fatigue, social withdrawal
Why Money Is the Biggest Stress Driver
Money worries consistently rank at the top of American stress lists, and the connection to broader economic trends is clear. The U.S. Bureau of Labor Statistics reported that inflation reached a four-decade high in 2022, and although rates have cooled somewhat since then, prices for groceries, rent, and healthcare remain stubbornly high.
Even modest increases in the cost of living can push financially fragile households into constant anxiety mode.
The APA notes that financial stress does more than make people feel uneasy; it can directly affect physical health. People under long-term financial pressure often delay doctor’s appointments, skip preventive care, or cut back on medications to save money.
This creates a vicious cycle where stress worsens health, and poor health increases financial strain.
Work Stress and the Burnout Epidemic
American work culture is another major contributor to the stress epidemic. The American Institute of Stress estimates that 83% of U.S. workers experience work-related stress, and about half say they need help learning how to manage it.
The problem isn’t confined to high-pressure industries like finance or healthcare; retail, education, and service jobs report similar patterns of burnout and emotional fatigue.
Remote work, which many hoped would reduce stress, has created its own challenges. Blurred boundaries between work and personal life mean people are “always on,” answering emails late at night and skipping breaks.
Younger workers in particular are reporting high burnout rates: according to Gallup, about 68% of Gen Z and younger millennials say they feel burned out frequently, compared to about 40% of baby boomers.
The Physical Toll of Chronic Stress
Chronic stress is more than a mental strain – it physically changes the body over time. The APA and the National Institute of Mental Health (NIMH) point to increased risks for heart disease, hypertension, digestive issues, and weakened immune response.
Stress also worsens sleep quality, and sleep deprivation in turn amplifies stress, creating another damaging cycle.
A 2022 study published in JAMA Psychiatry found that individuals experiencing high stress over a prolonged period were two times more likely to develop metabolic syndrome, a cluster of conditions including high blood pressure, high blood sugar, and excess abdominal fat, all of which increase cardiovascular risk.
Generational Differences: Who Feels It Most?
Age Group
Most Common Stressors
Distinctive Trends
Gen Z (18–26)
Job insecurity, climate anxiety, debt, and cost of living
Highest rates of reported anxiety symptoms
Millennials (27–42)
Work-life balance, childcare costs, and the housing market
Significant burnout in mid-career
Gen X (43–58)
Health concerns, retirement readiness
Often caring for both children and aging parents
Baby Boomers (59+)
Health expenses, fixed income pressures
Slightly lower stress overall, but higher health-related anxiety
Younger adults often feel the squeeze from unstable job markets, student debt, and the cost of starting families, while older adults face stress tied to health and financial stability in retirement. Each generation experiences stress differently, but no group is untouched.
Why the Political and Social Climate Adds Fuel to the Fire
Beyond personal and financial challenges, the U.S. political and social landscape contributes to the strain. The APA has reported a marked increase in stress related to political division, social justice debates, and constant exposure to bad news. In 2023, about 55% of adults said the political climate was a significant stressor, up from 46% just a few years earlier.
This kind of ambient societal stress is harder to control because it’s tied to events outside an individual’s direct influence. The nonstop news cycle and social media make it nearly impossible to disconnect, meaning stressors can feel constant.
A Human Reality Behind the Numbers
Statistics give us the scale of the problem, but they don’t capture the lived experience: the parent cutting back on groceries to pay for a child’s medical bill, the worker lying awake at night before a performance review, or the recent graduate wondering how they’ll ever afford rent.
The APA’s findings underline the importance of acknowledging these pressures openly. The stigma around talking about stress has been fading, which is encouraging, but access to affordable mental health care remains uneven.
Catching Mental Health Issues Before They Escalate
One reason stress remains such a widespread and persistent issue in the United States is that many underlying mental health conditions go undetected or misdiagnosed. According to Creyos, misdiagnosis rates as high as 65.9% for major depressive disorder, 92.7% for bipolar disorder, and 71.0% for generalized anxiety disorder (Vermani et al., 2011).
Without accurate screening, stress can mask the symptoms of these conditions, delaying effective treatment and prolonging suffering.
Behavioral health assessments – ranging from brief self-report questionnaires to comprehensive cognitive evaluations – offer a structured way for healthcare providers to distinguish between general stress and diagnosable disorders.
This not only improves treatment accuracy but also helps prevent mild conditions from progressing into more severe mental health crises.
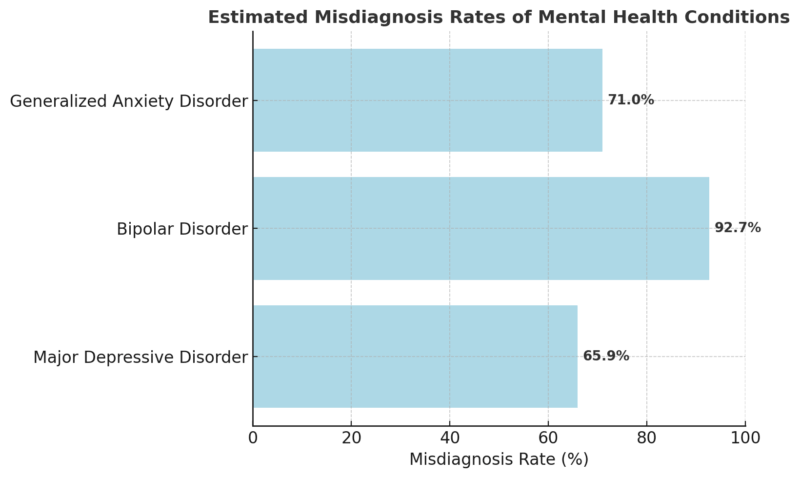
By integrating accurate, validated screening tools into routine health visits, providers can address the mental health component of stress early – potentially reducing the national burden of chronic stress-related illness.
Methodology
This article was developed using a synthesis of reputable public data sources, including surveys from the American Psychological Association, Gallup, and the American Institute of Stress.
We reviewed the most recent nationwide statistics on stress levels, causes, and demographic differences, ensuring all figures came from recognized research bodies. Information was organized into thematic sections: financial stress, workplace burnout, health effects, generational differences, and societal factors, to create a clear and logical flow.
Tables were included to present quantitative findings in an accessible format.
Final Word
@drrebeccaheiss Every American is dealing with 3 MAJOR stresses in their life. Here is how to fix that. 👆🏼 #fearless #lifetips #lifelessons #lifelesson #lifecoach #lifecoaching #stress #stressrelief #stressed ♬ Stardust – Hotel Pools
Stress in America is not a passing problem; it’s a structural issue that’s tied to economics, culture, and public policy. The latest reports make one thing clear: managing stress isn’t just a personal responsibility, it’s a societal one.
Solutions need to address the root causes, affordable healthcare, financial stability, and healthier work environments – rather than relying solely on individual coping strategies.
For now, individuals can take practical steps, setting boundaries at work, seeking social connection, practicing regular physical activity, and, when possible, accessing mental health services.
But long-term improvement will require bigger changes. Until then, the story of stress in America remains one we’re all living together – whether we talk about it or not.
Related Posts:
- 39% of Gen Z Say AI Would Be a Better Boss Than a…
- Why Everyday Sounds Like Chewing and Breathing Can…
- A Groundbreaking Eye Treatment Just Restored Vision…
- Dermatologists Say Millions Over 65 Are Showering…
- A Tiny Gut Molecule Might Cut Type 2 Diabetes Risk,…
- Experts Say This Ancient Gene Is Making Pain Feel Worse