Statin use has evolved significantly over the years as more awareness about cardiovascular health and cholesterol management has grown.
The data from 1988–2008 and subsequent years paints a clear picture of this growth in statin prescriptions, particularly in the U.S. adult population aged 45 and above.
Below, We provide a comprehensive analysis of the numbers shown in your image (1988–2008), as well as a detailed look at trends from 2008 to 2018, based on available research.
Table of Contents
ToggleStatin Use from 1988–2008 (%)
Year Group
Age Group
Total (%)
Men (%)
Women (%)
1988–1994
45 years and over
2.4
2.3
2.6
45–64 years
0.9
0.9
0.9
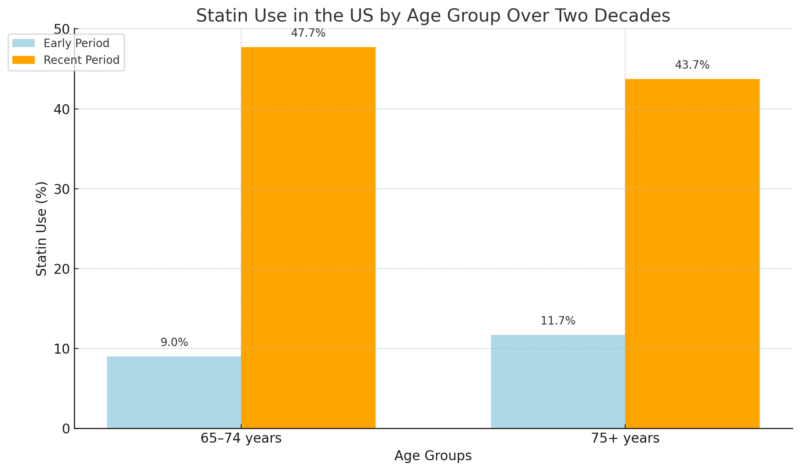
65–74 years
9.0
8.1
9.6
75 years and over
11.7
9.7
13.1
1999–2002
45 years and over
11.1
12.6
9.9
45–64 years
6.9
7.3
6.5
65–74 years
29.9
31.0
29.1
75 years and over
33.9
33.3
34.4
2005–2008
45 years and over
23.4
24.9
22.0
45–64 years
16.1
16.7
15.4
65–74 years
47.7
48.1
47.4
75 years and over
43.7
46.2
41.6
Overall Increase
Statin use rose from 2.4% (1988–1994) to 23.4% (2005–2008) for adults aged 45 and over. This growth reflects a significant shift in medical practice, where statins became widely prescribed as evidence of their benefits for cardiovascular disease prevention accumulated.
Age Differences
Older adults (65+) saw the most dramatic increase in statin use:
Gender Differences
Men consistently had higher statin use across the periods, likely due to a higher risk for heart disease. By 2005–2008, 24.9% of men aged 45+ were using statins, compared to 22.0% of women.
Statin Use from 2011–2018 (%)
Year Group
Age Group
Total (%)
Men (%)
Women (%)
2011–2012
40 years and over
27.8
29.4
26.3
40–64 years
23.9
25.1
22.7
65 years and over
70.8
71.9
69.7
2018
40 years and over
19.9
22.7
17.1
40–64 years
16.8
18.4
15.2
65 years and over
58.1
60.2
56.0
Continued Increase, but Slower Growth
By 2011–2012, statin use had reached nearly 27.8% among adults 40 and over, showing a consistent rise, though the growth rate slowed after the surge seen in the early 2000s.
However, there was a slight decline in the use by 2018 to 19.9%, likely influenced by updated cholesterol guidelines in 2018 that refined the criteria for statin recommendations according to CDC Stacks.
Age Groups

- In 2011–2012, nearly 70.8% of adults aged 65 and older were using statins, demonstrating that this older demographic remains a key focus for cholesterol management. This number slightly reduced to 58.1% by 2018, possibly due to stricter guidelines that recommended fewer older adults without cardiovascular disease be prescribed statins
- In contrast, adults aged 40–64 had a lower and more stable statin use rate, with 23.9% in 2011–2012 and 16.8% in 2018.
Gender Differences
In 2011–2012, 29.4% of men used statins compared to 26.3% of women. This difference remained consistent through 2018, where 22.7% of men used statins, versus 17.1% of women.
These differences may stem from men’s higher historical risk of cardiovascular disease, though statin use among women has been increasing in line with new research indicating its benefits across genders as per JAMA Network notes.
Use of the PREVENT equations was associated with fewer US adults being eligible for primary prevention statin therapy; however, the majority of adults eligible for receiving such therapy based on PREVENT equations did not report statin use. https://t.co/wJxnCM1uxa pic.twitter.com/YBex0u19Ow
— JAMA Internal Medicine (@JAMAInternalMed) August 21, 2024
Aging Population and Cardiovascular Risk
View this post on Instagram
A post shared by GEHA – Government Employees Health Association (@gehahealth)
As the U.S. population continues to age, statins have remained central to managing cardiovascular risk, particularly for adults over 65. The rise in statin use, especially among the elderly (70.8% in 2011–2012), reflects both the prevalence of heart disease in older populations and the acceptance of statins as a primary therapeutic intervention.
Even as the guidelines were adjusted in 2018, which led to a slight reduction in overall statin use, these drugs continue to play a vital role in the prevention of cardiovascular events like heart attacks and strokes.
Amro Matyori notes that:
“Statins are the drugs of choice in treating hyperlipidemia and preventing or reducing heart diseases. In 2013, the American College of Cardiology (ACC) and the American Heart Association (AHA) revised the Adult Treatment Panel III (ATP-III) guidelines to minimize the risk of cardiovascular diseases (CVD), which dramatically have increased the number of people eligible to take statins. The previous protocols targeted patients diagnosed with CVD or diabetes and low-density lipoprotein (LDL) cholesterol level of ≥ 100 mg/dL. In addition, the ATP-III protocols indicated statins for primary prevention in individuals based on LDL cholesterol profile and the 10-year risk of coronary heart disease (CHD) using the Framingham risk formula.”
Guideline Changes and Their Impact
The 2018 Cholesterol Guidelines made significant changes to statin recommendations. These guidelines emphasized personalized risk assessments over blanket statin prescriptions for certain age groups, particularly those without overt cardiovascular disease.
This led to a slight reduction in statin use, especially among older adults and low-risk individuals. For instance, statin use among adults aged 65 and over dropped from 70.8% in 2012 to 58.1% in 2018.
These changes represent a more targeted approach to treatment, aiming to reduce unnecessary statin use while focusing on those at high risk.
Gender and Racial Disparities

Statin use is higher among men than women, a trend that has remained consistent across decades.
This may be attributed to historically higher cardiovascular disease rates in men.
However, gender disparities in statin use are narrowing as women, especially those at risk of cardiovascular diseases, are increasingly prescribed statins.
Furthermore, disparities based on racial and ethnic groups persist, with lower statin use observed among Hispanic, Black, and Asian populations.
Efforts to address these disparities are needed to ensure that all high-risk groups have access to cholesterol-lowering therapies.
Methodology
The article was based on a comprehensive review of data from national health surveys and relevant studies. The National Health and Nutrition Examination Survey (NHANES) and the Centers for Disease Control and Prevention (CDC) data from 1988–2018 were used to highlight trends in statin use among U.S. adults aged 40 and over.
Comparative analysis across different years (1988–2008, 2011–2018) helped show the rise in statin prescriptions, while insights from additional sources such as JAMA Network and NCBI provided context on demographic differences, cholesterol guidelines, and statin usage across various age groups and genders.
Key steps included:
- Data Collection: Reviewing NHANES and CDC reports.
- Comparative Analysis: Analyzing statin use trends over different decades.
- Integration of Guidelines: Highlighting the impact of evolving cholesterol treatment guidelines on statin prescriptions.
References:
- CDC – Statistics on Statin Use
- JAMANETWORK – National Trends in Statin Use and Expenditures in the US Adult Population From 2002 to 2013
- Matyori A, Brown CP, Ali A, Sherbeny F. Statins utilization trends and expenditures in the U.S. before and after the implementation of the 2013 ACC/AHA guidelines. Saudi Pharm J. 2023 Jun;31(6):795-800. doi: 10.1016/j.jsps.2023.04.002. Epub 2023 Apr 11. PMID: 37228328; PMCID: PMC10203693.