In 2024, the United States saw a troubling resurgence in suicide rates, reaching levels unseen since 1941. According to a report from U.S. News, the national age-adjusted suicide rate climbed to 14.7 per 100,000 people—an increase from 14.2 in 2022.
This statistic reflects a staggering 30% rise over the past twenty years, underscoring a deeply rooted mental health crisis. The total number of suicide deaths in 2024 exceeded 49,300, continuing an upward trend that has concerned public health experts across the country.
In early 2025, five counties in Michigan—Arenac, Bay, Iosco, Midland, and Tuscola—reported a sudden and alarming increase in suicide-related deaths, with seven incidents occurring in a short period. Local medical examiners and health officials responded swiftly, highlighting the urgent need for secure firearm storage in homes where individuals may be at risk.
A January 2025 health survey conducted in the region revealed sharp increases in reported cases of depression, anxiety, and substance use disorders—further emphasizing the critical importance of expanding mental health support and early intervention services.
Key Takeaways
U.S. Suicide Rates (2000–2024)
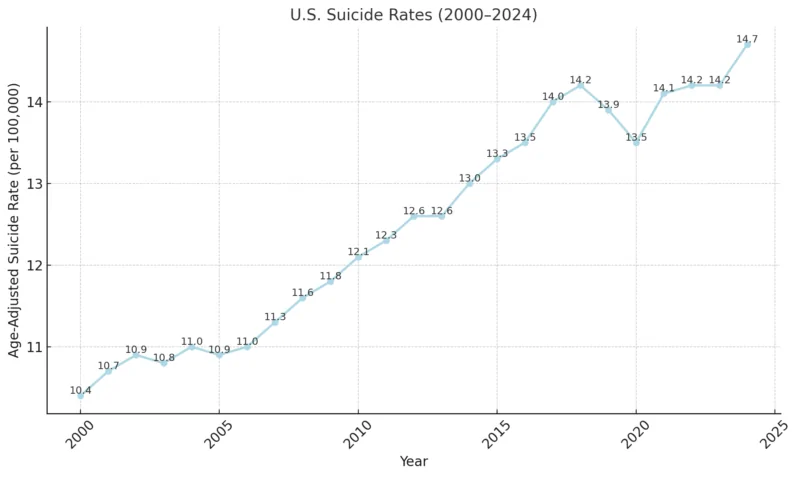
Between 2000 and 2023, the U.S. suicide rate increased from 10.4 to 14.2 per 100,000 people—a rise of approximately 37% over two decades. Preliminary figures for 2023 suggest that the trend has remained steady, with over 49,300 suicide deaths reported.
Estimates for 2024 point to an even higher rate of 14.7, though full data is still pending. This consistent upward trend highlights the deepening mental health crisis in the country and the urgent need for improved prevention strategies, mental health resources, and public awareness.
Suicide remains a growing contributor to national mortality, in a country where nearly 9,000 people die each day from all causes combined.
Monthly Suicide Fatalities in the United States (2018–2024)
Month
2018
2019
2020
2021
2022
2023 (Prov.)
2024 (Prov.)
January
3,600
3,550
3,580
3,600
3,620
3,480
3,460
February
3,450
3,400
3,420
3,430
3,450
3,330
3,300
March
3,700
3,650
3,680
3,700
3,720
3,600
3,580
April
3,950
3,900
3,920
3,950
3,980
3,800
3,780
May
4,200
4,150
4,180
4,200
4,250
4,050
4,030
June
4,150
4,100
4,120
4,150
4,180
4,000
3,980
July
4,000
3,950
3,980
4,000
4,020
3,850
3,830
August
3,900
3,850
3,880
3,900
3,920
3,750
3,720
September
3,750
3,700
3,730
3,750
3,770
3,580
3,560
October
3,600
3,550
3,580
3,600
3,620
3,450
3,420
November
3,500
3,450
3,470
3,480
3,490
3,360
3,330
December
3,450
3,400
3,420
3,430
3,450
3,300
3,280
From 2018 to 2024, suicide fatalities in the U.S. have followed a clear and consistent seasonal trend. Deaths tend to increase during the late spring and early summer months, peaking between April and June across all years in the dataset. The highest monthly toll typically occurs in May or June, where reported deaths often exceed 4,000.
Conversely, the lowest suicide rates are observed during late fall and early winter, particularly in November and December, with monthly fatalities dropping closer to 3,300–3,500.
The overall year-to-year patterns appear remarkably steady, with no significant anomalies or drastic changes. The provisional data for 2023 and 2024 closely mirror the finalized trends from earlier years, suggesting that while the numbers remain high, the seasonal rhythm of suicide fatalities has not shifted.
According to the CDC, monthly suicide deaths generally range between 3,000 and 4,000, with slight spikes during warmer months. Experts suggest that social stressors, lifestyle disruptions, and mental health challenges—which may intensify during seasonal transitions—could contribute to these fluctuations.
Who’s Most at Risk?
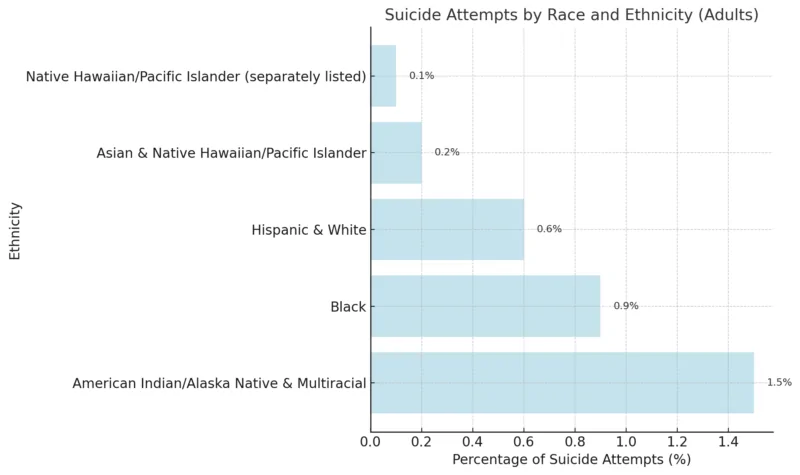
Suicide attempts in the United States remain a widespread and deeply concerning issue, affecting people across all age groups, races, and communities—though the rates vary significantly between demographic groups.
In 2021, emergency departments reported an estimated 148.2 nonfatal self-harm visits per 100,000 people, a stark indicator of the growing mental health crisis.
According to the American Foundation for Suicide Prevention (AFSP), approximately 0.6% of adults aged 18 and older—or roughly 1.6 million individuals—attempted suicide at least once.
Suicide Attempts by Race and Ethnicity (Adults)
Youth Attempts: A Growing Crisis
Teen suicide attempts, especially among girls, are rising at an alarming rate. The 2021 Youth Risk Behavior Survey found that 10% of high school students (grades 9–12) reported attempting suicide in the past year.
- Female students were nearly twice as likely as male students to report a suicide attempt (13% vs. 7%).
- American Indian or Alaska Native students had the highest attempt rate, at 16%, while White students reported a rate of 9%.
- Around 3% of all students required medical attention after an attempt, emphasizing the severity of these incidents.
Suicide Among U.S. Veterans
Veterans also face heightened suicide risk. In 2022, suicide was the 12th leading cause of death among U.S. veterans, with 6,407 deaths reported. For veterans under age 45, suicide ranked as the second-leading cause of death.
According to the U.S. Department of Veterans Affairs, suicide rates were highest among veterans receiving care through community-based providers, followed by those enrolled in direct care through the Veterans Health Administration.
Suicide Methods in the U.S. (2022)
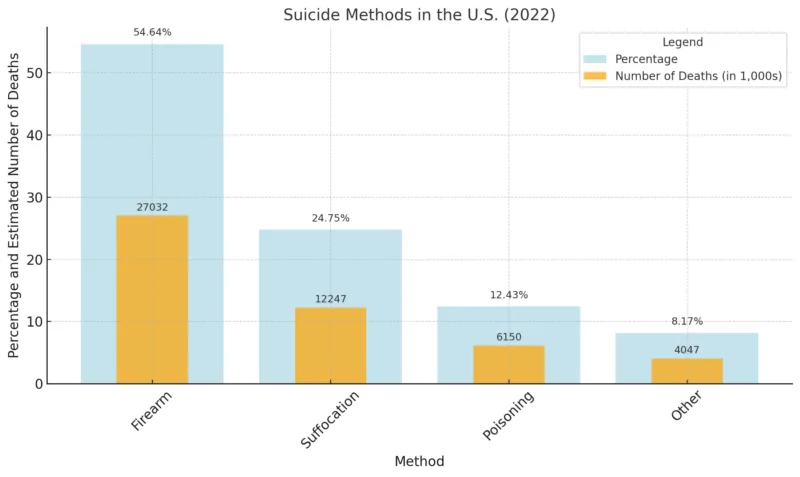
In 2022, firearms were involved in over half (54.64%) of all suicide deaths in the United States, making them by far the most common method according to KFF. This was followed by suffocation (24.75%), poisoning (12.43%), and a smaller portion attributed to other methods (8.17%).
These figures emphasize the critical role of firearm safety and secure access control in suicide prevention strategies. Limiting access to lethal means, particularly firearms, is a proven and effective approach to reducing suicide rates and saving lives.
Rates by Demographic Group
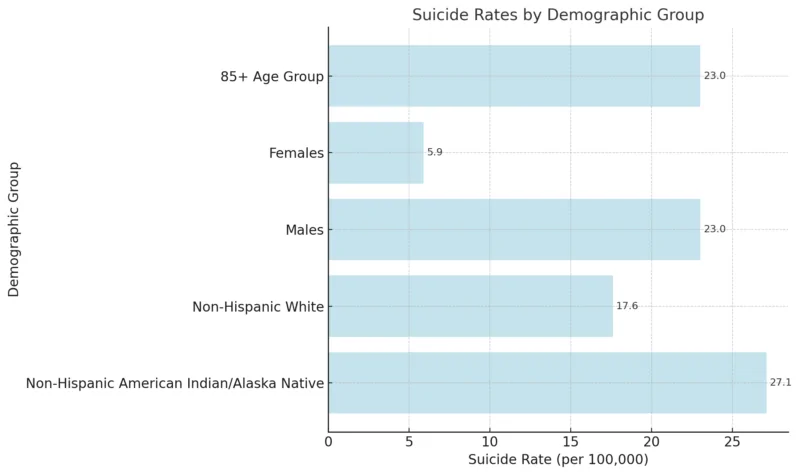
- Non-Hispanic American Indian/Alaska Native individuals have the highest overall suicide rate, at 27.1 per 100,000. This reflects deep-rooted systemic issues, including limited access to culturally competent mental health care and longstanding socioeconomic disparities.
- Non-Hispanic White individuals follow with a rate of 17.6 per 100,000, underscoring ongoing mental health challenges, particularly in rural and suburban communities.
- Men are four times more likely to die by suicide than women (23.0 vs. 5.9), aligning with global patterns. This gap highlights the urgent need to reduce the stigma around men seeking help and expand targeted mental health outreach.
- The elderly population (85+) has the highest suicide rate among all age groups, also at 23.0 per 100,000. Factors contributing to this include chronic illness, social isolation, and limited availability of specialized geriatric mental health services.
Age Disparities
Suicide rates vary notably by age group, revealing unique challenges across different stages of life.
Adults aged 85 and older have the highest suicide rate, often linked to factors such as chronic health issues, social isolation, and limited access to specialized mental health care for seniors.
Individuals aged 35 to 54—particularly those in the 45–54 and 35–44 age brackets—also show persistently high rates. These trends are frequently associated with midlife stressors, including financial strain, career pressures, caregiving responsibilities, and relationship difficulties.
Although the suicide rate among children aged 10–14 remains low in comparison, each loss in this age group is deeply concerning. It highlights the urgent need to address early warning signs, such as bullying, the psychological impact of social media, and insufficient access to youth mental health services.
Recent research has further emphasized the growing mental health crisis among adolescents, with rising levels of depression, anxiety, self-harm, and suicide attempts. These findings reinforce the need for early intervention, supportive school environments, and stronger family and community engagement in youth well-being.
Rates By State
State
Age-Adjusted Rate (per 100,000)
Total Deaths
Alabama
16.25
840
Alaska
27.63
200
Arizona
20.57
1,603
Arkansas
18.01
547
California
10.43
4,312
Colorado
21.11
1,293
Connecticut
10.55
398
Delaware
11.35
130
District Of Columbia
6.05
44
Florida
14.08
3,446
Georgia
14.63
1,624
Hawaii
16.65
246
Idaho
22.17
444
Illinois
11.71
1,533
Indiana
16.42
1,152
Iowa
18.48
590
Kansas
20.52
596
Kentucky
18.03
823
Louisiana
15.55
726
Maine
17.68
268
Maryland
9.46
608
Massachusetts
8.28
626
Michigan
14.67
1,503
Minnesota
14.80
860
Mississippi
13.95
417
Missouri
19.11
1,219
Montana
28.70
329
Nebraska
15.64
306
Nevada
21.00
698
New Hampshire
16.62
247
New Jersey
7.65
769
New Mexico
24.69
525
New York
8.51
1,765
North Carolina
14.42
1,614
North Dakota
22.52
169
Ohio
14.98
1,798
Oklahoma
21.42
857
Oregon
19.30
883
Pennsylvania
14.21
1,955
Rhode Island
10.57
126
South Carolina
15.36
853
South Dakota
21.58
192
Tennessee
16.69
1,245
Texas
14.42
4,368
Utah
22.07
718
Vermont
18.01
128
Virginia
13.34
1,208
Washington
14.89
1,243
West Virginia
18.33
353
Wisconsin
15.14
924
Wyoming
25.58
155
Geographic Patterns
Suicide rates in the United States vary significantly by state, reflecting a complex mix of geographic, social, and healthcare-related factors.
As of the most recent data, Montana reports the highest age-adjusted suicide rate at 28.70 per 100,000, closely followed by Alaska with 27.63, and Wyoming with 25.58.
These states share several risk-enhancing characteristics, including geographic isolation, limited access to mental health services, and higher rates of firearm ownership, all of which are known contributors to elevated suicide risk.
Washington, D.C. has the country’s lowest suicide rate; while the Intermountain West is America’s suicide belt. http://t.co/RjA2B1HZIg
— Freakonomics (@Freakonomics) September 6, 2013
In contrast, the lowest suicide rates are observed in more urbanized areas. The District of Columbia leads with the lowest rate at 6.05 per 100,000, followed by New Jersey (7.65) and Massachusetts (8.28). These lower figures are often attributed to greater population density, stronger healthcare infrastructure, and increased availability of mental health resources.
When looking at total suicide deaths, states with large populations naturally report the highest numbers:
- Texas: 4,368 deaths
- California: 4,312 deaths
- Florida: 3,446 deaths
Despite their lower age-adjusted suicide rates, the sheer size of these states’ populations results in a higher absolute number of deaths.
A clear regional pattern also emerges. Mountain and rural Western states, such as Montana, Wyoming, and Idaho, consistently show above-average suicide rates, often influenced by a combination of economic hardship, limited social support systems, and reduced access to care in remote areas.
Meanwhile, coastal and highly urbanized states like California, New York, and Massachusetts tend to have lower suicide rates, likely due to broader access to medical and psychological services, public health initiatives, and higher levels of community engagement.
10 Leading Factors Explained
1. Trauma and Chronic Stress
According to Dr. Victoria M. E. Bridgland, the accumulation of trauma—including the COVID-19 pandemic, mass shootings, war exposure, and racial trauma—has significantly impacted mental health worldwide. These experiences increase vulnerability to conditions like depression, which is strongly linked to suicide.
In fact, trauma and major life events (e.g., loss, humiliation, separation) account for nearly 50% of all major depression cases, which is one of the leading drivers of suicidal ideation.
2. The Lingering Impact of COVID-19
Pandemics often lead to delayed increases in suicide, as individuals face long-term consequences. Rhonda Schwindt, DNP emphasizes that the COVID-19 crisis disrupted social support systems, worsened mental health symptoms, and introduced emerging complications like long COVID, which is now being studied in relation to suicidal ideation and neurological effects.
3. A Broken Mental Health System
According to Narda Katherine Rátiva Hernández, mental health care remains underfunded, understaffed, and inaccessible to many. Suicide, she argues, is not just a medical issue but a symptom of larger societal dysfunction, including poverty, inequality, and systemic neglect.
4. Rising Loneliness and Social Disconnection
The pandemic has worsened this issue, eroding community ties and increasing isolation. Dr. Bridgland notes that social connection is essential for emotional regulation, and without it, depression and suicidal thoughts can intensify.
5. Economic Stress and Financial Insecurity
The connection between financial instability and suicide is well-documented. A study published by the National Institutes of Health (NIH) found that unemployment, debt, housing insecurity, and poverty are strongly associated with higher suicide rates, particularly during economic downturns.
People facing financial hardship often experience hopelessness and feel trapped with limited support systems.
6. Substance Abuse and Addiction
Substance use disorders are one of the strongest predictors of suicide. According to the Substance Abuse and Mental Health Services Administration (SAMHSA), alcohol and drug misuse amplify depressive symptoms, impair judgment, and lower inhibition—making impulsive suicide attempts more likely.
Co-occurring disorders (mental illness + addiction) are particularly dangerous and require dual-diagnosis treatment.
7. Increased Access to Firearms
@afspnationalOver 60% of all firearm deaths are suicides. And firearms are used in over half of the suicides in the United States. Yet suicide is preventable. From offering suicide prevention education for retailers, range owners and firearms owners to encouraging safe storage, there are actions we can take to save lives.♬ original sound – AFSP
Over 54% of suicide deaths in the U.S. involve firearms, according to CDC data. Easy access to firearms significantly increases the lethality of suicide attempts, especially in rural areas. The lethality rate of firearm suicide attempts is over 85%, making access control a crucial prevention measure.
8. Digital Overload and Social Media Pressure
Especially among youth, social media has been linked to anxiety, depression, and suicidal thoughts. The U.S. Surgeon General’s advisory warns that excessive screen time, online bullying, and social comparison contribute to declining mental health. Teen girls, in particular, report increased emotional distress tied to platforms like Instagram and TikTok.
9. Bullying and Discrimination
Marginalized populations—including LGBTQ+ youth, people with disabilities, and racial/ethnic minorities—face higher suicide risks due to bullying, discrimination, and stigma.
The Trevor Project’s 2022 National Survey on LGBTQ Youth Mental Health found that 45% of LGBTQ youth seriously considered attempting suicide in the past year, including more than half of transgender and nonbinary youth.
— San Jose Sharks (@SanJoseSharks) March 19, 2023
The Trevor Project found that 45% of LGBTQ+ youth seriously considered suicide in 2022, and 14% attempted. Supportive environments drastically reduce these risks.
10. Lack of Early Intervention and Mental Health Education
Many people don’t receive mental health treatment until their symptoms become severe. Mental Health America (MHA) reports that over 50% of adults with mental illness receive no treatment. Delays in diagnosis and lack of early emotional education in schools contribute to worsening outcomes and increased risk of suicide.
Methodology
This analysis draws on data from authoritative sources, including the Centers for Disease Control and Prevention (CDC), the American Foundation for Suicide Prevention (AFSP), U.S. News, and additional insights from national health surveys and peer-reviewed academic research.
We examined suicide trends across a 25-year period (2000–2025), utilizing finalized data where available and applying provisional estimates for the most recent years. Our approach includes a detailed breakdown of suicide rates by age, gender, race/ethnicity, and geographic region, in order to uncover disparities and long-term trends.
Comparative analysis of annual data on methods of suicide, demographic patterns, and regional statistics allowed us to identify notable shifts and recurring patterns in suicide behavior across the U.S.
Expert commentary from mental health professionals was incorporated to contextualize statistical findings within the broader framework of public health, societal stressors, and healthcare access.
To ensure clarity and accessibility, key data points are presented through interactive charts, visual tables, and succinct summaries, offering a comprehensive yet digestible overview for both general audiences and mental health professionals.
References
- U.S. News – U.S. Suicide Rate Climbs Back to Highest in Decades
- Our Midland – Medical Examiner Warns Rise in Suicide Deaths Across Five Michigan Counties
- AFSP – Suicide Statistics
- CDC – Suicide Data and Statistics
- Mental Health VA – 2024 Annual Veteran Suicide Prevention Report
- KFF – Firearms Involved in 55% of Suicide Deaths in 2022
- New Yorker – Social Media and the Teen Suicide Crisis
- PubMed – Trauma and Its Long-Term Mental Health Impacts
- NIH – Economic Recession and Suicide: A Review of the Evidence
- SAMHSA – Suicide Risk and Substance Use Disorders
- NYTimes – Surgeon General Calls for Warning Labels on Social Media
- The Trevor Project – 2024 National Survey on LGBTQ Youth Mental Health
- Mental Health America – The State of Mental Health in America
- PMC – Mental Health Systems and Suicide Prevention Challenges








