From 1950 to 2024, life expectancy in the United States has seen a substantial rise, evolving from an average of around 68 years to just over 79 years.
This growth signifies improvements in healthcare, lifestyle, and overall mortality rates over the decades.
In 2024, the life expectancy in the U.S. is projected to be approximately 79.25 years, according to Macrotrends.
Projections indicate a modest increase in the coming years, with life expectancy expected to reach around 79.3 years in 2025.
Key Takeaways
Timeline of U.S. Life Expectancy
Trends from 1950 to 1975
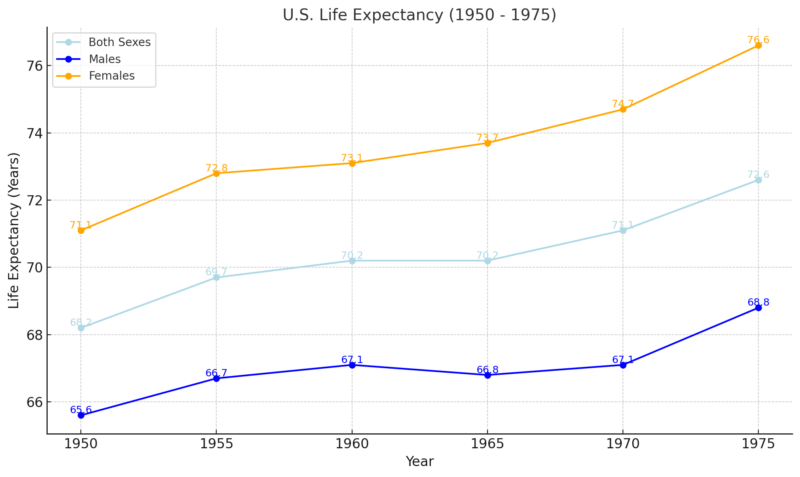
Between 1950 and 1975, life expectancy in the United States steadily increased, reflecting advancements in medical care, public health, and living conditions. Life expectancy at birth rose from 68.2 years to 72.6 years, an increase of 4.4 years over 25 years, averaging a growth of 0.18 years annually.
Gender differences were notable. Male life expectancy increased by 3.2 years, from 65.6 to 68.8 years, while females experienced a larger gain, rising from 71.1 to 76.6 years, an increase of 5.5 years. This disparity reflects greater advancements in women’s health, such as improved maternal care and chronic disease management.
The 1950s saw moderate growth, driven by vaccines, antibiotics, and post-WWII health infrastructure, while 1960 to 1975 saw continued improvement due to public health campaigns, reduced smoking rates, and Medicare’s introduction.
This period highlighted the influence of socioeconomic and medical progress, particularly benefiting women and narrowing gender gaps in longevity, setting the stage for continued gains in life expectancy.
Advancements from 1976 to 2000
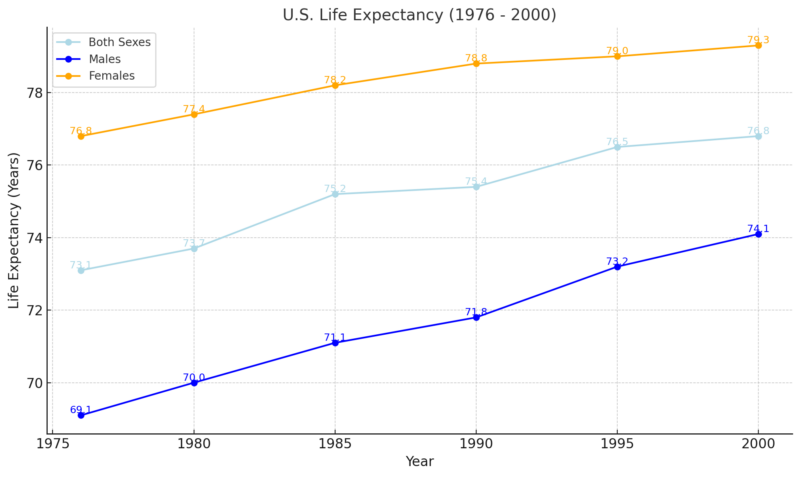
Medical advancements like heart disease and its treatments and cancer screenings contributed to increased survival rates.
Greater awareness and action against smoking also supported health improvements.
Despite advancements, the period faced challenges such as rising obesity rates and the HIV/AIDS epidemic, which disproportionately affected certain populations.
The HIV/AIDS Epidemic: Revisiting the Early Days of a Global Health Crisis
https://t.co/QirxARHAPt— GMHC (@GMHC) April 12, 2024
By 2000, life expectancy reached about 77 years, demonstrating continued, though sometimes uneven, progress.
Between 1976 and 2000, life expectancy in the United States continued to rise steadily, from 73.1 years to 76.8 years for both sexes.
This represents an increase of 3.7 years over 24 years, averaging approximately 0.15 years of growth annually.
The pace of improvement, while notable, was slightly slower than in the previous period from 1950 to 1975.
Gender Differences
Males experienced significant gains in life expectancy, increasing from 69.1 years in 1976 to 74.1 years in 2000, an increase of 5.0 years.
Female life expectancy grew more modestly, from 76.8 years to 79.3 years, an increase of 2.5 years.
This narrowing gender gap indicates improved health outcomes for men, likely due to reductions in smoking-related illnesses and better management of cardiovascular diseases, which historically impacted men more severely.
The 21st Century: 2001 to 2024
Year
Life Expectancy (Years)
Change (Years)
Percentage Change
2001
77.0
–
–
2002
77.0
0.0
0.00%
2003
77.2
+0.2
+0.26%
2004
77.6
+0.4
+0.52%
2005
77.6
0.0
0.00%
2006
77.8
+0.2
+0.26%
2007
78.1
+0.3
+0.39%
2008
78.2
+0.1
+0.13%
2009
78.5
+0.3
+0.38%
2010
78.7
+0.2
+0.25%
2011
78.7
0.0
0.00%
2012
78.8
+0.1
+0.13%
2013
78.8
0.0
0.00%
2014
78.9
+0.1
+0.13%
2015
78.7
-0.2
-0.25%
2016
78.6
-0.1
-0.13%
2017
78.7
+0.1
+0.13%
2018
78.8
+0.1
+0.13%
2019
78.9
+0.1
+0.13%
2020
78.99
+0.09
+0.11%
2021
78.99
0.0
0.00%
2022
79.05
+0.06
+0.08%
2023
79.11
+0.06
+0.08%
2024
79.25
+0.14
+0.18%
Between 2001 and 2024, life expectancy in the United States has shown a gradual upward trend. In 2001, the average life expectancy at birth was 76.90 years, increasing to 79.25 years by 2024. This represents an overall rise of approximately 2.35 years over the 23-year period.
The annual growth rate during this time has been modest, with year-to-year increases ranging from 0.03% to 0.26%.
The early 2000s experienced relatively higher annual increases in life expectancy, peaking at 0.26% between 2004 and 2006.
However, from 2015 onwards, the growth rate slowed, with annual increases hovering around 0.08%. Notably, in 2018, there was a slight decline of 0.03% compared to the previous year.
Several factors have influenced these trends. Advancements in healthcare, reductions in smoking rates, and improved treatments for diseases have contributed positively to life expectancy. Conversely, rising rates of obesity, substance abuse, and socioeconomic disparities have posed challenges.
The COVID-19 pandemic had a significant impact, causing a decline in life expectancy in 2020 and 2021.
However, there was a partial rebound in 2022, with life expectancy increasing by 1.1 years from 76.4 years in 2021 to 77.5 years in 2022, according to the CDC.
Despite these gains, the U.S. lags behind other developed nations in life expectancy. Projections indicate that by 2050, the U.S. could drop to 66th place globally, with an average life expectancy of 80.4 years. This decline is attributed to factors such as rising obesity rates and associated chronic diseases, as it is noted by the New York Post.
Determinants of Life Expectancy
Life expectancy in the U.S. is influenced by a variety of factors, which include genetics, healthcare quality, socioeconomic conditions, lifestyle choices, and environmental impacts. Each of these elements plays a critical role in shaping the average lifespan.
Genetic Factors
Research indicates that genetics accounts for approximately 20-30% of the variation in human lifespan, with the remaining 70-80% attributed to non-genetic factors.
Specific genetic components have been linked to longevity. For instance, certain variants of the APOE gene, particularly the APOE ε4 allele, are associated with an increased risk of Alzheimer’s disease and cardiovascular conditions, potentially reducing lifespan.
Carriers of the APOE ε4 allele may live approximately one year less per copy of the allele, primarily due to the heightened risk of Alzheimer’s disease.
Conversely, the FOXO3 gene has been identified as a positive contributor to longevity. Variations in FOXO3 are more frequently observed in individuals aged 100 and above, suggesting a protective effect against age-related diseases.
Healthcare Access and Quality
Health System Tracker notes that despite the United States’ high healthcare expenditure, outcomes often lag behind those of peer nations, partly due to unequal access to care.
In 2022, the U.S. spent nearly twice as much per capita on healthcare compared to other high-income countries, yet had a lower life expectancy than its peers.
This disparity is attributed to factors such as rising obesity rates, which are projected to affect over 260 million Americans by 2050, leading to increased chronic diseases like Type 2 diabetes and heart disease.
Additionally, the U.S. has the highest infant mortality rates and lowest life expectancy among high-income countries, despite its substantial healthcare spending.
These statistics highlight the critical need for improved healthcare access and quality to enhance life expectancy in the U.S.
Years of Life Lost During the COVID-19 Pandemic in the U.S. and Peer Countries (2020-2021).
Country
Under 50 Years (Total)
Under 50 Years per 100,000
Overall (<75 Years) (Total)
Overall (<75 Years) per 100,000
U.S.
4,842,384
2,034
9,412,234
3,139
U.K.
333,673
723
885,223
1,530
Germany
317,016
604
789,176
1,129
Canada
202,534
786
277,704
836
Sweden
16,953
239
43,983
498
Netherlands
39,998
344
55,678
371
France
119,353
279
167,443
306
Switzerland
15,437
263
18,107
243
Belgium
16,974
217
22,334
224
Austria
14,486
244
16,606
217
Japan
15,687
21
30,927
32
Socioeconomic Status
Economic disparities play a crucial role in life expectancy. Research indicates that individuals in the top 1% income bracket live significantly longer—14.6 years for men and 10.1 years for women—compared to those in the bottom 1% according to Equity Health Journal.
Additionally, a study from the University of California, Riverside, identified cumulative poverty as the fourth leading risk factor for mortality in the U.S., underscoring the profound impact of economic hardship on health outcomes.
Environmental Influences
A study published in the British Medical Journal found that long-term exposure to low levels of air pollution is associated with a substantial rise in mortality, even below current European and North American standards.
Climate change exacerbates these issues by increasing the frequency of extreme weather events, such as heatwaves and wildfires, which pose direct health risks.
The Centers for Disease Control and Prevention (CDC) notes that prolonged exposure to high temperatures can lead to heat-related illnesses and exacerbate chronic conditions like cardiovascular and respiratory diseases.
Additionally, environmental degradation disproportionately affects marginalized communities. Historical practices like redlining have resulted in certain neighborhoods experiencing higher levels of pollution and associated health problems.
Research indicates that life expectancy in redlined communities is, on average, 3.6 years lower than in non-redlined areas, with some cities exhibiting even larger disparities.
Impact of Chronic Diseases
Chronic diseases have significantly influenced U.S. life expectancy trends. Major factors include heart disease, stroke, cancer, diabetes, and respiratory diseases. These conditions have not only contributed to mortality rates but also affected the overall quality of life.
Heart Disease and Stroke

Cardiovascular diseases (CVD), including heart disease and stroke, are the foremost causes of death in the U.S. In 2021, CVD accounted for 931,578 deaths, surpassing fatalities from all forms of cancer and chronic lower respiratory diseases combined.
Despite advancements in medical treatments, the prevalence of risk factors such as high blood pressure, high cholesterol, and smoking continues to sustain high mortality rates.
Projections indicate that by 2050, at least 60% of U.S. adults could be affected by heart disease and stroke, potentially tripling related healthcare costs to $1.8 trillion according to the American Heart Association.
Cancer
Innovative public health strategies, such as prohibiting tobacco sales to specific age groups, could prevent significant numbers of cancer-related deaths.
For instance, banning tobacco sales to individuals born between 2006 and 2010 could avert 1.2 million lung cancer deaths worldwide over 70 years.
Diabetes
Diabetes affects approximately 11.3% of the U.S. population, equating to 37.3 million people. In 2021, diabetes was mentioned as a cause of death in 399,401 death certificates as it is noted by the American Diabetes Association.
The economic burden is substantial, with diagnosed diabetes costing $412.9 billion in 2022, including $306.6 billion in direct medical expenses and $106.3 billion in indirect costs.
Respiratory Diseases
CDC has noted that chronic lower respiratory diseases, including conditions like chronic obstructive pulmonary disease (COPD), accounted for 147,382 deaths in 2022, ranking as the sixth leading cause of death in the U.S.
Approximately 4.3% of adults have been diagnosed with COPD, emphysema, or chronic bronchitis.
These conditions not only contribute to mortality but also diminish the quality of life for those affected.
Recent Developments in U.S. Life Expectancy and Health Policies

The United States has implemented various public health initiatives and embraced technological advancements to enhance life expectancy. Despite these efforts, recent analyses indicate that the nation’s progress is lagging compared to other high-income countries.
Public Health Initiatives and Policies
The “Healthy People” program, initiated in 1979 by the U.S. Department of Health and Human Services, sets decade-long objectives to promote health and prevent diseases. The latest iteration, Healthy People 2030, emphasizes health equity, social determinants of health, and health literacy.
It aims to improve health and well-being across all life stages by focusing on measurable objectives and addressing upstream factors that influence health outcomes.
Despite such initiatives, the U.S. faces significant challenges. A 2024 report from the Bloomberg American Health Initiative revealed that the average life expectancy in the U.S. is 78.6 years, compared to 81.3 years in England and Wales.
This 2.7-year gap is primarily attributed to preventable causes such as heart disease, drug overdoses, firearm-related incidents, and motor vehicle crashes.
Technological Advancements in Healthcare

Since 1980, advancements in diagnostics, medical devices, procedures, and pharmaceuticals have contributed to a five-year increase in the average U.S. lifespan.
These innovations have led to earlier disease detection, improved treatment options, and better management of chronic conditions.
Wearable health technologies, such as fitness trackers and smartwatches, offer continuous health monitoring and data collection. However, their integration into standard healthcare practices has been slow.
Barriers include limited training for healthcare providers on data interpretation, high costs, and skepticism regarding the impact of such data on patient outcomes. Overcoming these challenges is essential to fully leverage wearable technology for health improvement.
Challenges and Future Directions
U.S. life expectancy is projected to rise modestly from 78.3 years in 2022 to 80.4 in 2050, with global rankings falling from 49th to 66th. #Healthcare #Health https://t.co/pQ0yi6wpGY
— Karina Martínez (@MtzTweets) December 6, 2024
Despite these efforts, the U.S. is projected to fall to 66th place globally in life expectancy by 2050, with an average lifespan of 80.4 years. This decline is largely due to a public health crisis driven by rising obesity rates, which increase the risk of chronic diseases like Type 2 diabetes, heart disease, and certain cancers.
To address these issues, experts recommend comprehensive strategies, including:
- Implementing evidence-based public health policies.
- Enhancing access to quality healthcare services.
- Promoting healthy lifestyles through education and community programs.
- Leveraging technological innovations for preventive care and disease management.
By adopting a multifaceted approach that combines effective public health initiatives with technological advancements, the U.S. can work towards improving life expectancy and overall population health.
Methodology
This article was crafted using a combination of historical data, official statistics, and research findings sourced from credible public health organizations, government reports, and academic studies. Recent insights on life expectancy trends were obtained from platforms like Macrotrends, CDC, and the American Heart Association.
Peer-reviewed journals and health-focused reports provided context for genetic, socioeconomic, and environmental determinants. Data on healthcare advancements and challenges were analyzed from sources like the Bloomberg American Health Initiative and time.com.
The impact of chronic diseases was explored through reports from the American Diabetes Association and CDC. Finally, public health initiatives and technological contributions were examined to highlight their role in shaping life expectancy trends.
References
- Macrotrends – United States Life Expectancy 1950-2024
- CDC – FastStats: Life Expectancy
- Health System Tracker – How Does the Quality of the U.S. Healthcare System Compare to Other Countries?
- Equity Health Journal – Cumulative Poverty and Mortality Risk in the U.S.
- University of California, Riverside – Poverty Is 4th Greatest Cause of U.S. Deaths
- BMJ – Long-Term Exposure to Air Pollution and Mortality
- American Heart Association – Heart Disease and Stroke Could Affect 60% of Adults by 2050
- American Diabetes Association – Statistics About Diabetes
- CDC – FastStats: Chronic Lower Respiratory Diseases
- Healthy People 2030 – U.S. Department of Health and Human Services
- Bloomberg American Health Initiative – Life Expectancy Years Shorter in the U.S. Compared to the U.K.
- Life Changing Innovation – Medical Technology Saves and Improves Lives
- New York Post – U.S. Expected to Drop to 66th Place in Life Expectancy Rankings