Despite years of attention and billions in funding, millions of Americans who want mental health treatment still aren’t getting it.
The most recent federal data (2023 NSDUH, released summer 2024) show that nearly one in four adults with any mental illness and over 40% of adolescents with depression said they needed mental health care but didn’t get it.
The top reasons are cost, stigma, not knowing where to go, and a persistent belief that they should handle things alone.
As 2025 begins, these gaps remain stubborn, especially for young adults and people in low-income or rural areas. New rules and policies aim to help, but the workforce shortage and insurance coverage issues mean that real progress is slow.
Who Needs Help, Who Gets It, and Who Doesn’t
8 in 10 cancer survivors have unmet needs 1-3yrs after treatment, including mental health needs. Partnerships are required to increase awareness and design solutions with cancer survivors, their families and caregivers, and cancer, mental health, primary care and labour sectors. pic.twitter.com/ra6ddguvQb
— Tanya Flanagan (@tanyaflanagan) June 7, 2020
The U.S. Substance Abuse and Mental Health Services Administration (SAMHSA) conducts the annual National Survey on Drug Use and Health (NSDUH), which remains the gold standard for this data. Here’s what the most recent results reveal:
Unmet Mental Health Needs by Age Group (2023 NSDUH)
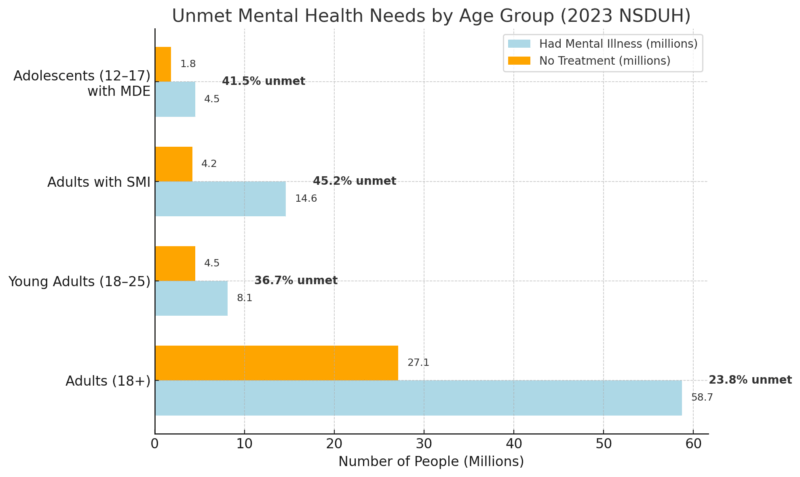
- Adults (18+): Of 58.7 million adults with any mental illness, 27.1 million did not receive treatment. About 6.2 million of those adults recognized they needed care but couldn’t get it, according to SAMHSA.
- Young Adults (18–25): This group consistently reports the highest unmet need, with nearly two million young adults saying they needed mental health treatment and didn’t receive it.
- Serious Mental Illness (SMI): The gap is even more severe. Nearly half of adults with SMI who went untreated said they had an unmet need; more than 1.9 million people.
- Adolescents: Among 1.8 million untreated teens with major depression, 749,000 reported they needed help but didn’t get it.
Main Barriers to Accessing Mental Health Care (Adults and Teens)
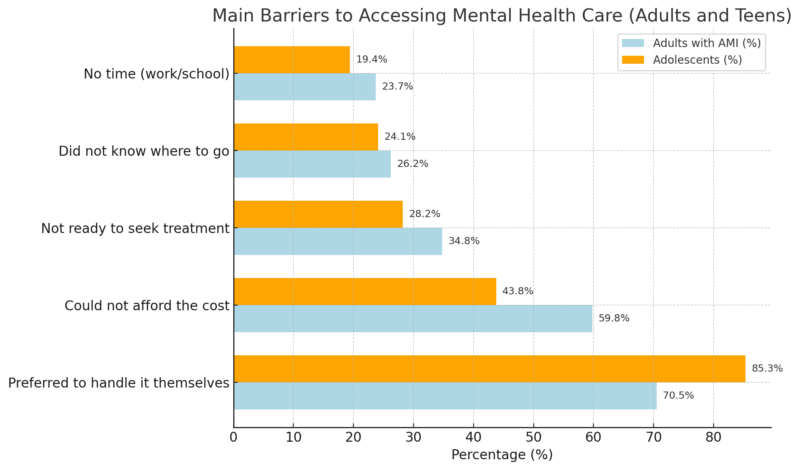
The single biggest barrier is the belief that “I should handle it myself”. This stigma and culture of self-reliance are deeply ingrained, especially in teens.
However, cost is the next most-cited reason, and it’s not just about having insurance; high copays, lack of in-network providers, and deductibles all play a role. A significant number of people simply don’t know where to start or don’t feel ready for treatment, while logistical hurdles like a lack of time also contribute.
Unmet Mental Health Need by Diagnosis Type
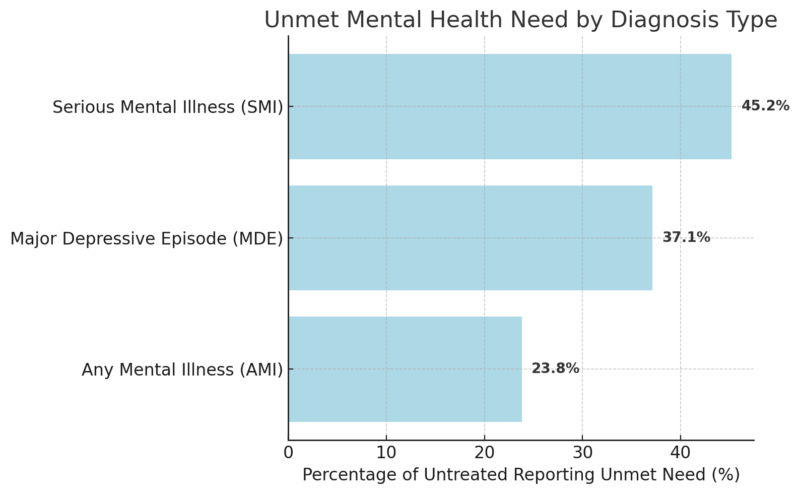
The severity of the mental health diagnosis directly affects how likely someone is to say they need help but are unable to get it. For any mental illness (AMI), a broad group that includes anxiety, mild depression, and other non-severe conditions, about 24% of untreated adults say they still recognize an unmet need for care.
This is already a concerning number given the prevalence of AMI in the U.S., where millions experience symptoms each year.
When looking specifically at major depressive episodes (MDEs), the percentage jumps to over a third. 37.1% of untreated people with depression acknowledge needing treatment as noted by NCBI, often involving prolonged sadness, loss of interest, and functional impairment.
Untreated depression is linked to increased risk of substance use, job loss, and even suicide, so this group is particularly vulnerable.
The situation is most critical for serious mental illness (SMI), which includes schizophrenia, bipolar disorder, and other severe, chronic conditions. Here, 45.2% of untreated individuals recognize an unmet need; almost half.
These individuals are at greater risk for homelessness, repeated hospitalization, and reduced life expectancy. Not only is the clinical burden higher, but the difficulty accessing specialized care is more pronounced. This means that, ironically, the people who need care the most are the ones most likely to go without it.
Provider Shortages and Workforce Trends (2025 Outlook)
Metric
Statistic/Trend
Psychiatrists accepting Medicare (2024)
Less than 50% in some regions
U.S. counties with severe MH provider shortage
Over 60% of counties
Americans with MI who didn’t get treatment (2024)
46%
Projected need for new mental health providers
25% increase needed by 2030
The national mental health workforce shortage is at crisis levels. Over 60% of U.S. counties (including rural areas and urban health deserts) simply do not have enough psychiatrists, therapists, or counselors to meet the mental health needs of their communities. In some areas, there is not a single practicing psychiatrist for hundreds of miles.
This shortage is particularly dangerous for older adults on Medicare. In some regions, less than half of psychiatrists accept new Medicare patients, which means seniors often go without needed care or are forced to seek help through emergency rooms and hospitals when issues escalate.
A 2024 Health Resources and Services Administration (HRSA) report highlighted that 46% of Americans with mental illness received no treatment at all; a number that has changed little despite increased awareness and funding. The reason is simple: there are not enough mental health professionals to meet the growing demand.
Projections suggest that by 2030, the country will need 25% more mental health providers just to keep pace with the current level of need, according to conventionspc.com. This includes psychiatrists, psychologists, social workers, and counselors.
The shortage is driven by retirement among current clinicians, burnout, insufficient new trainees, and uneven geographic distribution (with professionals clustering in major cities).
What’s Changing in 2025? Policy, Parity, and the Roadblocks That Remain
Area of Change
Description/Challenge
Mental health parity laws (MHPAEA)
New rules require insurance to cover MH services equally to physical health services
Workforce expansion efforts
Push for more providers, especially in shortage areas, and via telehealth
Insurance “ghost networks”
Many listed providers are unavailable or not accepting new patients
Cultural stigma
Persistent reluctance to seek care, especially among men and minorities
New parity rules under MHPAEA (Mental Health Parity and Addiction Equity Act) are designed to make insurance plans treat mental health and substance use coverage on par with physical health.
The intention is to lower out-of-pocket costs, remove arbitrary limits on therapy and psychiatric visits, and ensure equal access. If properly enforced, this could have a significant impact on how easily people can use their insurance for mental health care.
At the same time, there is a national push to expand the mental health workforce. This includes loan forgiveness for clinicians working in shortage areas, investment in training programs, and efforts to make telehealth services permanent.
Telehealth, in particular, has already shown promise in improving access for rural and mobility-limited populations.
However, it cannot fully solve the underlying shortage of trained professionals, especially for people needing in-person care or complex case management.
A significant barrier that remains is the phenomenon of “ghost networks”: insurance directories that list mental health providers who are either not taking new patients, have outdated contact information, or don’t accept the advertised insurance.
This makes it extremely difficult for patients to find care, even if they have insurance coverage. Many people spend weeks calling providers, only to be told they are not accepting new patients, leading to frustration and, often, people simply giving up.
Finally, cultural stigma continues to block access. Many Americans (especially men, older adults, and some ethnic communities) feel pressure to manage mental health struggles on their own due to shame, fear of discrimination, or cultural expectations.
This stigma is reflected in the top self-reported reason for not seeking care: the belief that one should “handle it themselves”.
The Human Impact of Unmet Need
Imagine a teenager who recognizes their depression but can’t afford a therapist, or a middle-aged adult juggling work and family who’s too embarrassed to ask for help. These are not rare cases; they are the norm for millions.
Data shows that untreated mental illness is linked to:
A single year of untreated depression can cost an individual more than $10,000 in lost earnings and medical bills, not to mention the toll on family and relationships.
Consequences of Unmet Mental Health Need
Consequence
Estimated National Impact
Lost productivity (2023 estimate)
$193 billion/year
Annual suicide deaths (2023)
49,500+
% of ER visits for a mental health crisis
~12%
Homeless population with SMI
Over 25%
When people can’t get the help they need, the entire country pays the price. Lost work, more ER visits, and even deaths; all are direct results of untreated mental illness.
Endnote
@lisah_muthoni Unmet needs make you vulnerable. Know your hunger or someone else will feed it for their benefit #healingjourney #trauma #mentalhealth #motivation #inspiration #therapy #fyp ♬ original sound – Muthoni /Mental wellness coach
America’s mental health care system is at a crossroads. The numbers show the need is immense, the barriers are well known, and while 2025 brings some policy progress, the real change will take time.
If you or someone you know is struggling, you’re not alone, and the fight for better access is far from over.
- At least six million adults and 750,000 teens wanted mental health care but didn’t get it last year.
- Cost, stigma, and provider shortages are the top obstacles.
- New laws and funding may help, but there’s no overnight fix, especially for those in rural, low-income, or minority communities.
For those seeking help, persistence is critical: check multiple providers, explore telehealth, and seek out community mental health resources. For policymakers and advocates, the mission is clear: reduce cost, build workforce, and attack stigma at every turn.
Related Posts:
- Health Insurance Coverage - National Health…
- The Rise of Suicide Rates in US - What 2024 Data…
- 8 Eye-Opening Statistics on Mental Health Disorders…
- How Lighting Affects Mental Focus, Sleep, and Eye Health
- Mental Health Trends Among Veterans – PTSD and…
- Stomach Cancer - Survival Rates and the Importance…








