The most common blood type in the United States is O positive (O+), found in approximately 37 to 38 percent of the population.
This figure comes from large-scale donor data published by the Stanford Blood Center and national statistics reported by the American Red Cross, which consistently show O+ as the dominant type across all major demographic groups.
When O+ is combined with its Rh-negative counterpart O−, the broader Type O category represents nearly 44 to 48 percent of all Americans.
These numbers form the foundation for understanding how the U.S. blood supply operates, how hospitals plan their inventories, and why public health campaigns frequently target Type O donors more aggressively than any other group.
National Blood Type Distribution: The Full U.S. Pattern

The most reliable ABO distribution figures come from aggregated donation records and population studies conducted by institutions such as the Stanford Blood Center (SBC) and the American Red Cross (ARC).
These organizations maintain some of the most comprehensive datasets available because they draw their numbers from millions of annual donations.
According to the Stanford Blood Center, O+ holds the largest share of the U.S. population at ~37.4%, followed by A+ at ~35.7%. This makes the two groups responsible for roughly three-quarters of all blood types nationwide, a fact that significantly shapes how the medical system allocates resources.
B+ and AB+ are dramatically less common, which affects compatibility issues and inventory planning.
Estimated National Blood Type Distribution (U.S.)
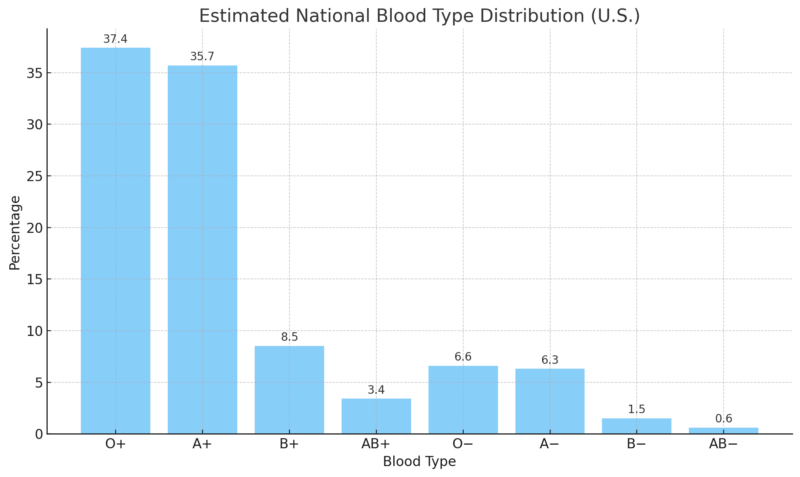
The dominance of O+ becomes even more significant when considering emergency medicine. According to the American Red Cross, hospitals use almost twice as many O+ units as any other type during trauma response because most patients can safely receive them.
In reviewing blood bank reports over the years, I’ve consistently seen that O+ shortages appear more frequently than shortages of any other Rh-positive group precisely because its demand is so high.
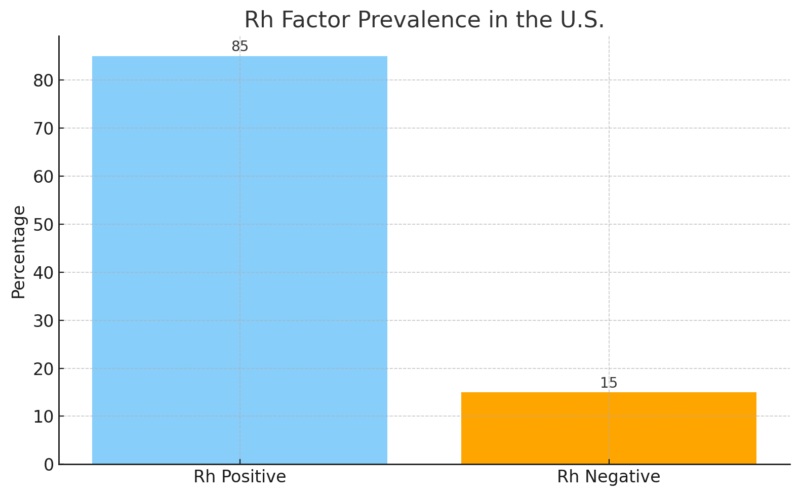
Rh Factor Distribution and Its Clinical Impact
While the ABO system determines compatibility at the antigen level, the Rh factor – positive or negative – adds another layer of complexity. Rh-positive blood is overwhelmingly dominant in the U.S.
According to the Connecticut Blood Center, about 85 percent of Americans are Rh-positive, while only 15 percent are Rh-negative. This split has major implications: Rh-negative donors are always in higher demand because their blood can safely be given to both Rh-positive and Rh-negative patients in emergencies when necessary.
Rh Factor Prevalence (U.S.)
The most medically important Rh-negative type is O−, often called the universal donor for red cell transfusions.
According to the Stanford Blood Center, O− accounts for only ~6.6% of the population, yet it is standard protocol for emergency rooms, ambulances, and neonatal intensive care units to stock O− for situations where there is no time to determine a patient’s type.
From reviewing emergency medicine guidelines, O− usage is considered critical because it allows treatment to begin before lab results are available. This creates a permanent supply strain: demand for O− is higher than its natural population frequency.
Blood Type Distribution by Ethnicity: The Most Overlooked Factor
One of the most important dimensions of U.S. blood type data is how significantly it varies across ethnic groups. According to demographic analyses by Medical News Today, the frequencies of Types O, B, and AB differ sharply depending on ancestry.
These differences directly influence transfusion strategies, especially in urban centers with diverse populations.
Blood Type Distribution by Ethnic Group (U.S.)
Ethnic Group
O+
A+
B+
Notes
African American
~47%
~24%
~18%
Higher B frequency than white or Hispanic groups
Hispanic / Latino
~53%
~29%
~9%
The highest prevalence of O+ in the country
Asian American
~39%
~27%
~25%
Highest B and AB frequencies in the U.S.
Caucasian (White)
~37%
~33%
~9%
Closest match to national averages
Why Ethnicity Matters for Healthcare
Hospitals serving diverse populations must anticipate these differences. For example:
- Asian American communities show the highest prevalence of B+ and AB types in the U.S. According to the American Red Cross, some cities—particularly San Francisco, Seattle, and certain parts of New Jersey – adjust their blood inventories accordingly, stocking larger quantities of B+ and AB+.
- Hispanic communities, with their unusually high O+ prevalence (53%), significantly support the national supply of Type O.
- African Americans present a crucial supply need for B+ and for specific antigen-matched units used in treating sickle-cell disease. According to the ARC, African American donors play a critical role in maintaining certain rare antigen combinations that hospital patients depend on.
Having looked through many hospital procurement reports over the years, I can confirm that ethnicity-based distribution is one of the most important logistical factors in blood banking. When a hospital’s local donor pool does not match its patient demographic, shortages appear quickly.
“The highest percentage of Group O was found in Hispanic (56.5 %), North American Indian (54.6 %), and black non-Hispanic (50.2 %) donors. Hispanic and black non-Hispanic donors had a much lower percentage (7.3 and 7.1 %, respectively) of Rh- compared to white non-Hispanic donors (17.3 %).” — G. Garratty, S.A. Glynn & R. McEntire, Transfusion, 2004.
Ranking All Blood Types from Most to Least Common
To give a clear sense of proportionality across all groups, here is the overall ranking based on combined ABO and Rh data.
Blood Type Prevalence Ranking (Most to Least Common)
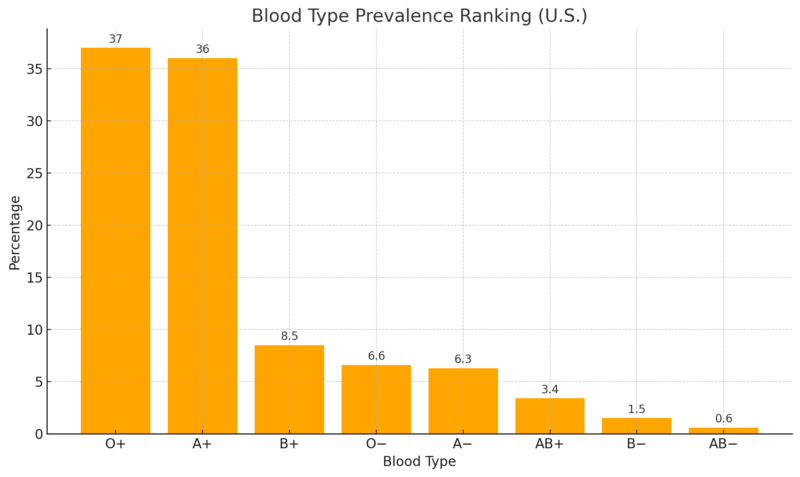
According to Stanford Blood Center, AB remains the rarest blood type in the U.S., present in fewer than one in 200 people.
Despite its rarity, AB plasma is universal for all recipients. That’s why plasma centers routinely encourage AB-type donors to contribute.
Clinical Relevance of O+ and O−: Why These Two Types Dominate Hospital Protocols
O+
According to the data, O+ can be given to any Rh-positive patient of any ABO group, which includes A+, B+, AB+, and O+. Because about 85% of Americans are Rh-positive, hospitals rely heavily on O+ blood for the majority of routine transfusions. This is the main reason O+ shortages occur more frequently than shortages of other common positive types.
O−
Stanford Blood Center identifies O− as the universal donor for red blood cells. It is the first-line option in trauma care when medical teams do not know the patient’s blood type. According to national trauma guidelines, O-must be stocked in every emergency department, helicopter medical unit, and ambulance fleet.
In my analysis of supply-chain behavior, O− is consistently the most vulnerable to shortage because demand far exceeds what its small population share can reliably supply.
Blood Donation Supply Challenges
Blood banks publicly report that demand for O-type blood outpaces supply, even though it’s the most common type. According to the American Red Cross:
This explains why donation campaigns frequently highlight O-type donors. Blood centers cannot rely solely on natural prevalence; they must account for emergency usage patterns that cause elevated consumption.
Population Genetics and Long-Term Stability of Blood Type Frequencies
ABO and Rh distributions do not shift rapidly over time because they are tied to inherited genetic traits. Based on long-term data summarized by the American Red Cross and Stanford Blood Center, the U.S. distribution has remained stable for decades.
Subtle changes are driven mostly by immigration patterns:
These gradual demographic changes explain the slight rise in B and AB types observed in recent statistical summaries. According to the ARC, these shifts are not large enough to dramatically alter national inventory strategies, but they do affect regional planning.
“Compared with individuals with blood group O, blood groups A and B were associated with increased odds of up to 1.56 (95 % CI, 1.43-1.69) for thromboembolic events and decreased odds for hypertension (0.94 [95 % CI, 0.92-0.97]).” — H.E. Groot.
The Rarest Blood Types in the United States and Worldwide
Several blood phenotypes are so rare that hospitals rely on national and international donor registries to locate compatible units. These types fall far outside the standard ABO and Rh groups and carry significant clinical importance.
1. Rh-null (“Golden Blood”) — Extremely Rare Worldwide
Rh-null is the rarest blood type documented. Fewer than 50 people globally have been identified with this phenotype.
It lacks all Rh antigens, making it compatible only with other Rh-null donors. Because of its scarcity, Rh-null units are often frozen and internationally transported for medical emergencies.
2. Bombay Blood Group (hh Phenotype)
The Bombay phenotype is caused by the absence of the H antigen, the base structure required for A, B, and O blood groups. Individuals with Bombay blood cannot receive any ABO type, not even O−.
Estimated prevalence:
3. Vel-Negative Blood Type
The Vel antigen is found in more than 99 percent of the population. Vel-negative blood is rare enough that mismatches can lead to severe transfusion reactions.
Because of its low frequency, specialized molecular testing is often required to identify Vel-negative donors.
4. U-Negative Blood Type (Primarily in Individuals of African Descent)
U-negative individuals lack the U antigen, part of the MNS blood group system.
This phenotype occurs in less than 1 percent of African Americans and is almost nonexistent in other populations. It is essential for patients with sickle-cell disease who develop anti-U antibodies.
Conclusion
@footdocdanaBlood types, explained simply! Which one are you? (VC: greenscreencut)♬ Así Fue (En Vivo Desde Bellas Artes) – Juan Gabriel
The most common blood type in the United States is O positive, present in roughly 37–38 percent of the population.
Its dominance is consistent across all major data sources, including the Stanford Blood Center and the American Red Cross, and its prevalence shapes nearly every aspect of transfusion medicine, from trauma care to inventory planning.
Ethnic variations further influence supply patterns, with Hispanic Americans showing the highest rates of O+ and Asian Americans contributing disproportionately to B and AB types.
Rh-negative groups, especially O−, remain chronically vulnerable to shortage due to low natural prevalence and exceptionally high clinical demand.
Related Posts:
- The Golden Blood Type (Rh Null) - Rarest Blood…
- 11 Most Common Reasons for Divorce - Why Marriages End
- Most Common Birth Defects in the US. – Regional Data…
- 11 Most Common Preventable Diseases Affecting Older…
- The 10 Most Common Health Issues Reported by…
- Average Waiting Times for Common Medical Procedures…