When doctors talk about cholesterol, most people immediately think of LDL or HDL. But in reality, the most reliable measure of your risk for heart disease is often non-HDL cholesterol. This number captures all the “bad” cholesterol types in your blood, not just LDL, and gives doctors a more complete picture of your cardiovascular health.
The concrete answer: For most adults, a healthy non-HDL cholesterol level is below 130 mg/dL. For children and teens under 19, the target is lower, under 120 mg/dL. Anything higher means there are too many plaque-forming lipoproteins circulating in the bloodstream, which increases the risk of atherosclerosis, heart attack, and stroke according to Medline.
Unlike LDL alone, non-HDL includes LDL, VLDL, IDL, and lipoprotein(a), making it a broader and often better predictor of future heart disease events.
Table of Contents
ToggleWhat Exactly Is Non-HDL Cholesterol?
Non-HDL cholesterol is calculated by subtracting your HDL (“good” cholesterol) from your total cholesterol.
Non-HDL=Total Cholesterol–HDL\text{Non-HDL} = \text{Total Cholesterol} – \text{HDL}Non-HDL=Total Cholesterol–HDL
It’s a way of capturing all the cholesterol particles that can lodge in arteries and form plaque. These particles include:
- LDL (low-density lipoprotein) – the main driver of artery-clogging plaque
- VLDL (very-low-density lipoprotein) – carries triglycerides and contributes to the buildup
- IDL (intermediate-density lipoprotein) – a transitional form between VLDL and LDL
- Lipoprotein(a) – a genetic cholesterol particle strongly linked to early heart disease
Because it includes more than just LDL, many cardiologists now view non-HDL as a stronger marker for risk assessment than LDL alone.
Average and Healthy Ranges
Here are the widely accepted ranges for non-HDL cholesterol:
Age Group
Optimal Non-HDL Level
Borderline High
High Risk
Children & Teens (≤19 yrs)
<120 mg/dL
120–144 mg/dL
≥145 mg/dL
Adults (20+ yrs)
<130 mg/dL
130–159 mg/dL
≥160 mg/dL
To put this into perspective:
Why Non-HDL May Be Better Than LDL Alone

Several studies show that non-HDL cholesterol predicts cardiovascular events more accurately than LDL:
- A 2020 JAMA study following more than 68,000 adults found that non-HDL levels were more strongly associated with risk of coronary heart disease than LDL levels, especially in people with high triglycerides.
- The Framingham Heart Study noted that individuals with normal LDL but high non-HDL were still at significant risk of heart disease.
- Guidelines from the European Society of Cardiology (ESC) recommend non-HDL as the primary target for lipid management in patients with metabolic syndrome or diabetes, since triglyceride-rich lipoproteins play a bigger role in these groups.
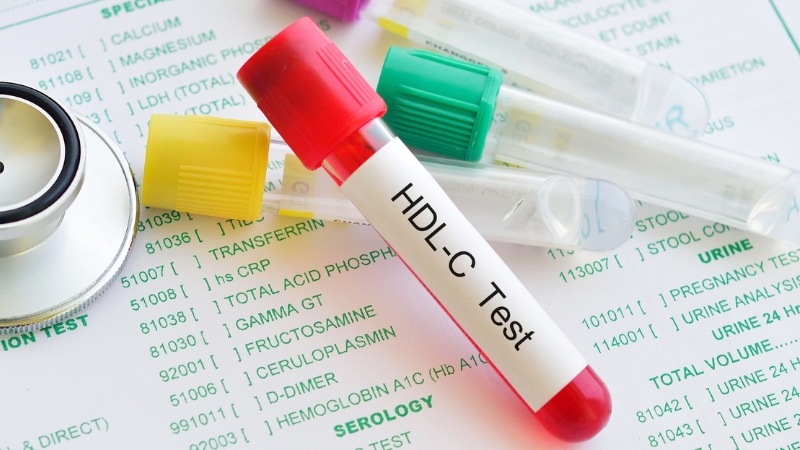
Cholesterol Test Components: How Non-HDL Fits In
When you get a lipid panel, you’ll usually see these numbers:
Marker
What It Means
Healthy Level
LDL
“Bad” cholesterol causes plaque buildup
<100 mg/dL
HDL
“Good” cholesterol removes fats from the blood
≥40 mg/dL (men), ≥50 mg/dL (women)
Total Cholesterol
Sum of HDL + LDL + other fractions
125–200 mg/dL
Triglycerides
Stored fat in blood, linked to VLDL
<150 mg/dL
Non-HDL
Total minus HDL measures all harmful particles
<130 mg/dL
If your lipid panel doesn’t list non-HDL, you can calculate it in seconds using the formula above.
Risk Factors for High Non-HDL Cholesterol
High non-HDL cholesterol does not happen overnight. It is the result of a combination of lifestyle habits, underlying medical conditions, and in some cases, genetics.
What makes non-HDL particularly concerning is that even when LDL cholesterol looks “normal,” elevated triglycerides or VLDL can drive non-HDL higher, putting people at greater cardiovascular risk.
Lifestyle-Related Risks
One of the strongest drivers of elevated non-HDL cholesterol is diet. Diets rich in saturated fats and trans fats—commonly found in red meat, fried food, baked goods, and processed snacks – lead to an excess of triglyceride-rich lipoproteins in the blood. Over time, these particles accumulate in artery walls, fueling atherosclerosis.
Obesity and metabolic syndrome are also closely linked to higher non-HDL. In particular, people with central obesity (fat around the waist) tend to produce more triglycerides, which directly raise VLDL and non-HDL levels.
Similarly, individuals with type 2 diabetes often have a dangerous lipid pattern known as atherogenic dyslipidemia: high triglycerides, low HDL, and elevated non-HDL.
Other major lifestyle contributors include smoking, which damages arterial walls and lowers HDL, and excessive alcohol consumption, which raises triglyceride levels. Finally, a sedentary lifestyle compounds these risks, as physical inactivity reduces HDL and worsens fat metabolism.
Genetic Risks
Not all cases of high non-HDL cholesterol are explained by lifestyle alone. Genetics can play a powerful role.
A key example is elevated lipoprotein(a), or Lp(a), a genetically determined lipoprotein that behaves like LDL but is far more atherogenic. Individuals with high Lp(a) often see higher non-HDL levels despite leading otherwise healthy lifestyles.
Risk Factor
Impact on Non-HDL Cholesterol
Mechanism
High intake of saturated/trans fats
Increases LDL, VLDL
Promotes liver production of harmful lipoproteins
Obesity / Metabolic syndrome
Raises triglycerides and VLDL
Insulin resistance leads to fat buildup in the blood
Type 2 diabetes
Increases triglycerides, lowers HDL
Causes atherogenic dyslipidemia pattern
Smoking
Lowers HDL, increases plaque buildup
Damages artery walls, accelerates atherosclerosis
Alcohol overuse
Raises triglycerides and VLDL
Excess calories are converted into blood fats
Sedentary lifestyle
Decreases HDL, raises non-HDL
Reduced fat metabolism efficiency
Genetics (e.g., Lp(a))
Raises non-HDL regardless of lifestyle
Hereditary lipoprotein abnormalities
How to Lower Non-HDL Cholesterol

The good news is that non-HDL cholesterol responds well to intervention. In many cases, lifestyle changes alone can bring levels back into a healthy range, particularly if detected early.
For people at high cardiovascular risk, medications can provide additional protection.
Lifestyle Changes
Diet remains the cornerstone of cholesterol control. Shifting away from saturated and trans fats toward a diet rich in whole foods makes a measurable difference, according to NCBI.
Increasing soluble fiber – found in oats, legumes, fruits, and vegetables – helps remove cholesterol from the bloodstream. At the same time, reducing fried and processed foods prevents the liver from producing excess LDL and VLDL.
Exercise is equally powerful. The American Heart Association recommends at least 150 minutes of moderate aerobic activity per week. Regular movement improves HDL levels, lowers triglycerides, and reduces the pool of harmful lipoproteins that contribute to non-HDL cholesterol.
Weight management is another proven tool. Research shows that losing just 5–10% of body weight can improve cholesterol ratios and lower both LDL and non-HDL.
Finally, cutting back on alcohol and quitting smoking has direct benefits. Alcohol is calorie-dense and easily converted into triglycerides, while smoking damages arteries and reduces HDL. Addressing both habits lowers cardiovascular risk even before cholesterol numbers change.
Medical Treatments
How does a statin reduce cholesterol?
Medical Doctor: Statin drugs lower cholesterol by slowing down the liver’s production of cholesterol. They also increase the liver’s ability to remove cholesterol that is already in the blood. Their mode of action is primarily through the… pic.twitter.com/Dd7aQa7OR2
— TheLiverDoc™ (@theliverdr) August 23, 2023
If lifestyle adjustments aren’t enough, doctors often prescribe medications. Statins are the most common, lowering LDL but also improving non-HDL levels.
Other options include ezetimibe, which blocks cholesterol absorption, and PCSK9 inhibitors, powerful injectables that significantly reduce LDL and total non-HDL cholesterol.
Intervention
Effect on Non-HDL Cholesterol
Evidence/Notes
A diet rich in fiber, fruits, vegetables, and whole grains
↓ LDL, ↓ VLDL
Proven to reduce cholesterol absorption and improve lipid ratios
Exercise (≥150 min/week)
↓ Triglycerides, ↑ HDL
Improves fat metabolism and heart health
Weight loss (5–10% body weight)
↓ Non-HDL, ↑ HDL
Even modest loss improves cholesterol balance
Limit alcohol
↓ Triglycerides
Reduces VLDL and non-HDL
Quit smoking
↑ HDL, ↓ arterial damage
Improves vessel health and cholesterol ratios
Statins
↓ LDL & ↓ Non-HDL
First-line therapy, well-studied
Ezetimibe
↓ Non-HDL
Blocks the absorption of dietary cholesterol
PCSK9 inhibitors
Strong ↓ LDL & Non-HDL
Used in high-risk patients or statin-intolerant cases
Screening Guidelines
Doctors recommend regular cholesterol screening:
Those with heart disease, diabetes, or multiple risk factors may need more frequent checks.
Methodology
This article was crafted using data from authoritative sources, including the National Heart, Lung, and Blood Institute (NHLBI), the American Heart Association (AHA), and peer-reviewed studies in journals such as JAMA.
We reviewed current clinical guidelines on cholesterol management and synthesized evidence about non-HDL cholesterol as a cardiovascular risk marker. Key numbers and ranges were taken directly from established medical references and cross-checked with multiple health databases.
Bottom Line
Non-HDL cholesterol is one of the best predictors of heart health because it includes all the harmful particles beyond LDL. A healthy target is under 130 mg/dL for adults and under 120 mg/dL for youth.
If your number is higher, it doesn’t always mean medication right away, but it does mean it’s time to take action. Lifestyle changes, diet, and regular screening can keep your numbers in check and lower your risk of heart attack or stroke.