The year 2017 marked a significant period for public health in the United States, as mortality rates showed troubling trends, especially regarding life expectancy and death rates across various demographics.
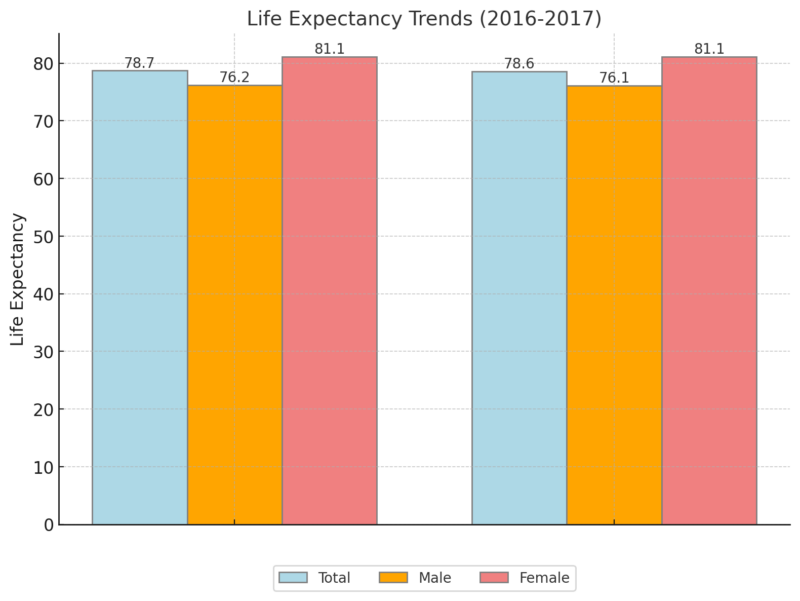
According to the National Vital Statistics System (NVSS), the overall life expectancy for the U.S. population fell slightly to 78.6 years, down from 78.7 years in 2016 (Murphy et al., 2018).
Although this decrease may seem marginal, it signals a broader public health crisis tied to issues like rising drug overdose deaths, increasing suicide rates, and persistent chronic diseases.
Table of Contents
ToggleThe Decline in Life Expectancy – What Does It Mean?
Life expectancy is one of the most critical indicators of a nation’s health, and the decline in 2017 was driven by increases in deaths from drug overdoses, suicides, and certain chronic illnesses.
As Sherry L. Murphy and her colleagues from the National Center for Health Statistics noted, the U.S. saw a notable drop in male life expectancy, from 76.2 years in 2016 to 76.1 years in 2017.
For females, life expectancy remained constant at 81.1 years (Murphy et al., 2018).
The gender disparity in life expectancy also widened slightly, with women expected to live 5.0 years longer than men, compared to 4.9 years in 2016.
These trends reflect ongoing health challenges, particularly among men, who are more likely to die from drug overdoses and suicide than women.
Rising Death Rates
The age-adjusted death rate for the total U.S. population increased by 0.4%, rising from 728.8 deaths per 100,000 people in 2016 to 731.9 per 100,000 in 2017 as per CDC notes.
This shift highlights the significant challenges facing public health officials, especially given the marked increases in death rates among specific age groups.
For instance, age-specific death rates rose by:
- 2.9% for those aged 25-34,
- 1.6% for those aged 35-44,
- 1.4% for those aged 85 and over (Murphy et al., 2018).
On the other hand, the death rate for the age group 45-54 decreased by 1.0%, which suggests some improvement in health outcomes for this demographic.
As noted by Darcy Jones McMaughan these fluctuations are often tied to socioeconomic factors, access to healthcare, and lifestyle choices, such as diet and exercise.
Causes of Death – What’s Driving Mortality?
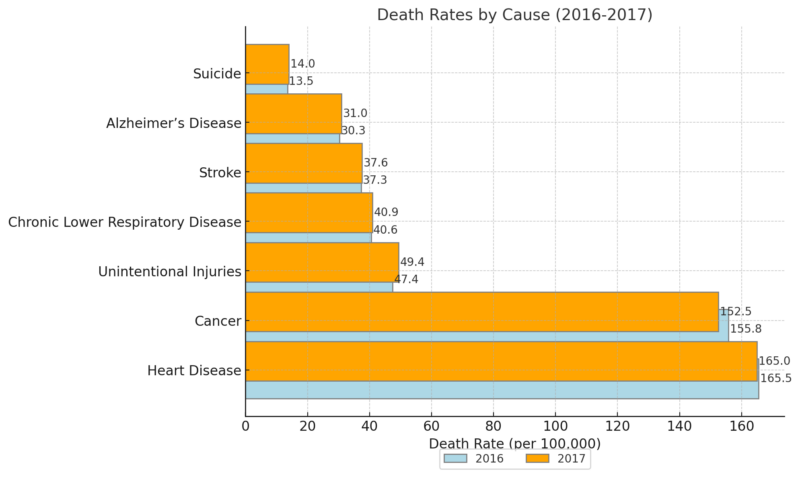
The leading causes of death in 2017 remained consistent with previous years, with heart disease and cancer continuing to dominate.
These two diseases alone accounted for a significant portion of all U.S. deaths, underscoring the need for ongoing research and better prevention strategies.
However, notable shifts occurred within the ranking of the top ten causes of death.
Unintentional injuries—driven primarily by the opioid epidemic—saw the most considerable rise, with a 4.2% increase in death rates from 47.4 deaths per 100,000 in 2016 to 49.4 per 100,000 in 2017.
As noted by Wayne R Lawrence, the rising death rates for unintentional injuries, largely due to drug overdoses, and suicide are alarming and demand immediate attention from policymakers and healthcare providers.
These two causes have become leading contributors to the overall decline in life expectancy, particularly among younger age groups.
The Opioid Crisis and Drug Overdose Deaths
One of the most pressing public health crises in recent years has been the opioid epidemic, which has dramatically increased the number of deaths due to drug overdoses.
In 2017, there were 70,237 drug overdose deaths, representing a 9.6% increase from 2016. The age-adjusted rate of drug overdose deaths was 21.7 per 100,000 people, up from 19.8 per 100,000 in 2016.
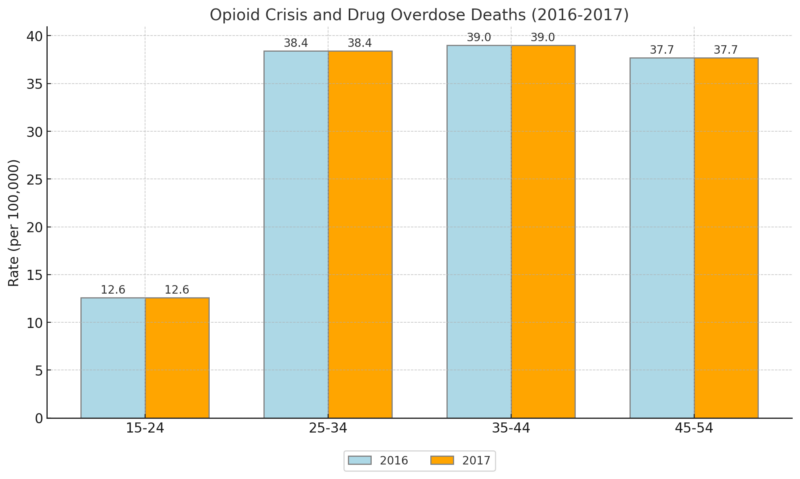
According to Dr. Holly Hedegaard, much of this increase can be attributed to synthetic opioids such as fentanyl and fentanyl analogs, which accounted for a 45% rise in overdose deaths from 2016 to 2017.
West Virginia, Ohio, and Pennsylvania had the highest drug overdose death rates, with West Virginia leading at 57.8 per 100,000 people (Hedegaard et al., 2018).
Suicide Rates
#NationalSuicidePreventionMonth: #Suicide is the third leading cause of death for 15-to 24-year-olds. https://t.co/rHamqGKYIY pic.twitter.com/4YmfAXO9iN
— Mental Health America (@MentalHealthAm) September 2, 2017
Suicide has become a major public health issue in the U.S., with the age-adjusted suicide rate increasing by 33% between 1999 and 2017. In 2017, the rate reached 14.0 per 100,000, up from 10.5 per 100,000 in 1999.
Men continue to die by suicide at higher rates than women, with males recording a rate of 22.4 per 100,000 compared to 6.1 per 100,000 for females.
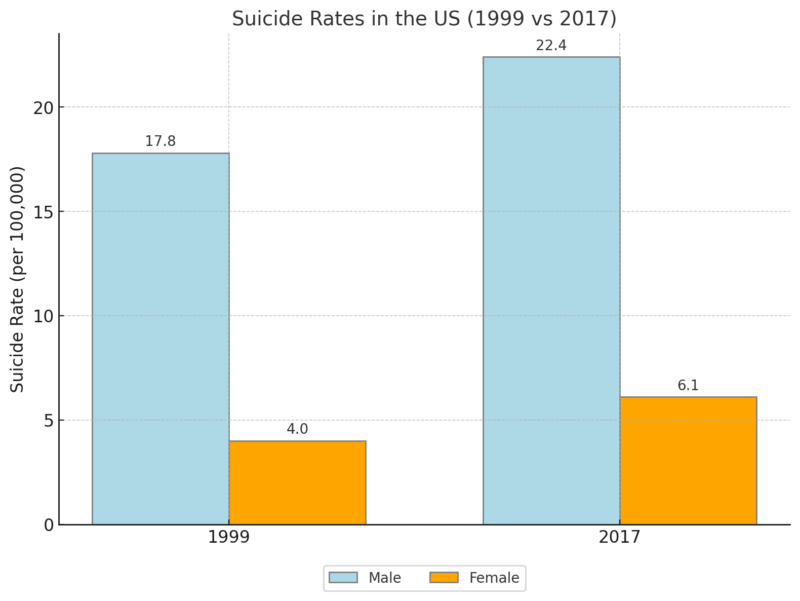
Dr. Margaret Warner pointed out that suicide rates were highest among men aged 75 and over, with a rate of 39.7 per 100,000, and among women aged 45-64, with a rate of 9.7 per 100,000.
Rural areas also saw a significant disparity in suicide rates compared to urban areas, with rural counties recording rates 1.8 times higher than those in urban centers (Hedegaard et al., 2018).
Infant Mortality – A Slight Decline
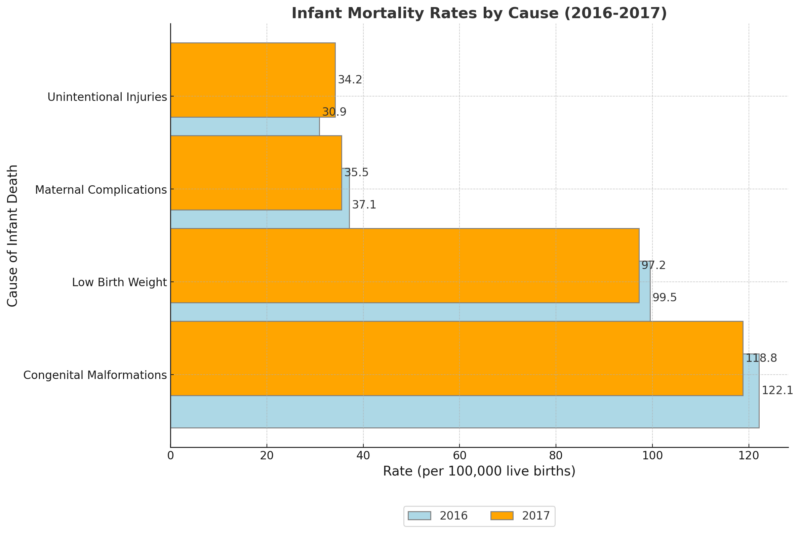
The infant mortality rate (IMR) in the U.S. decreased slightly in 2017, falling from 587.0 deaths per 100,000 live births in 2016 to 579.3 per 100,000. However, this decline was not statistically significant.
The leading causes of infant death remained largely unchanged, with congenital malformations, low birth weight, and maternal complications continuing to dominate. Unintentional injuries, however, showed a troubling 10.7% increase in infant mortality rates (Murphy et al., 2018).
Conclusion
The mortality data from 2017 highlight several critical public health challenges facing the United States. Life expectancy declined, driven by increases in deaths from drug overdoses, suicides, and chronic illnesses.
The gender disparity in life expectancy persisted, and rural communities continued to struggle with higher rates of suicide.
Addressing these issues requires a multifaceted approach, including better mental health services, stronger opioid addiction prevention programs, and continued research into chronic diseases.
As Sherry L. Murphy and her colleagues concluded, the path forward will depend on public health initiatives that prioritize prevention, early intervention, and equitable access to healthcare across all populations.
References
- Hedegaard H, Curtin SC, Warner M. Suicide mortality in the United States, 1999–2017. NCHS Data Brief, no 330. Hyattsville, MD: National Center for Health Statistics. 2018.
- Murphy SL, Xu JQ, Kochanek KD, Arias E. Mortality in the United States, 2017. NCHS Data Brief, no 328. Hyattsville, MD: National Center for Health Statistics. 2018.
- Lawrence WR, Freedman ND, McGee-Avila JK, Berrington de González A, Chen Y, Emerson MA, Gee GC, Haozous EA, Haque AT, Inoue-Choi M, Jackson SS, Lord B, Nápoles AM, Pérez-Stable EJ, Vo JB, Williams F, Shiels MS. Trends in Mortality From Poisonings, Firearms, and All Other Injuries by Intent in the US, 1999-2020. JAMA Intern Med. 2023 Aug 1;183(8):849-856. doi: 10.1001/jamainternmed.2023.2509. PMID: 37399025; PMCID: PMC10318548.
- Singh GK, Yu SM. Infant Mortality in the United States, 1915-2017: Large Social Inequalities have Persisted for Over a Century. Int J MCH AIDS. 2019;8(1):19-31. doi: 10.21106/ijma.271. PMID: 31049261; PMCID: PMC6487507.
- Arias E, Xu JQ. United States life tables, 2017.National Vital Statistics Reports; vol 68 no 7. Hyattsville, MD: National Center for Health Statistics. 2019.
- Murphy SL, Xu JQ, Kochanek KD, Arias E. Mortality in the United States, 2017. NCHS Data Brief, no 328. Hyattsville, MD: National Center for Health Statistics. 2018.
- Sherry L. Murphy, Jiaquan Xu, Kenneth D. Kochanek, and Elizabeth Arias are with the National Center for Health Statistics, Division of Vital Statistics.
- McMaughan DJ, Oloruntoba O, Smith ML. Socioeconomic Status and Access to Healthcare: Interrelated Drivers for Healthy Aging. Front Public Health. 2020 Jun 18;8:231. doi: 10.3389/fpubh.2020.00231. PMID: 32626678; PMCID: PMC7314918.