PTSD treatments in America are working for many people in 2025, but full recovery remains complex. Trauma-focused therapies like CBT and EMDR show 85% response rates with around 40% full remission, while advanced therapies such as vagus nerve stimulation and AI-enhanced neurofeedback are pushing remission rates even further in some trials.
Medications and combined therapies continue to help, while emerging trends such as psychedelic-assisted therapies and VR exposure therapy are reshaping the field.
Despite these advancements, barriers like cost, availability, and dropout rates remain obstacles for many seeking consistent care. However, for those who can access structured, trauma-focused therapy with or without advanced adjuncts, meaningful symptom reduction and even full remission are often within reach.
Table of Contents
TogglePTSD Treatment Success Rates at a Glance
Treatment Modality
Response Rate
Full Remission Rate
Notable Notes
Trauma-Focused Therapy (CBT, EMDR)
~85%
~40%
20% dropout rate
Medications (SSRIs, SNRIs)
62% improve
~42% (veterans)
Often combined with therapy for better outcomes
DBT + Prolonged Exposure (VA)
91%
—
Major symptom reductions reported
Vagus Nerve Stimulation (VNS)
85%
40%
Used adjunctively with CBT
AI-Neurofeedback (Prism)
67%
33%
Drug-free neurofeedback promising in trials
VR Exposure Therapy (VRET)
—
—
Matches in-person exposure effectiveness
Psychedelic-Assisted Therapy (MDMA)
—
—
Early studies show high potential pending FDA review
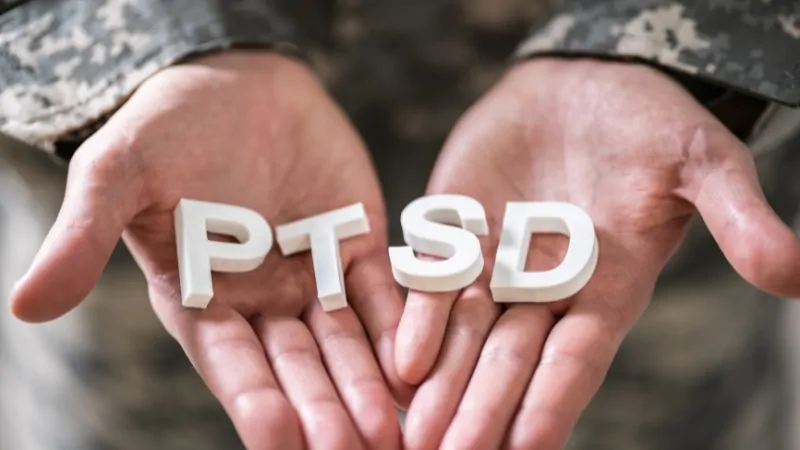
Post-traumatic stress disorder (PTSD) affects approximately 9 million Americans in 2025, with about 6% of adults experiencing it at some point in their lives. According to the NCBI, about 3.6% report past-year symptoms, with women (5.2%) more likely to be affected than men (1.8%).
Among veterans, 7% are living with PTSD, with many experiencing severe symptoms affecting daily life, relationships, and physical health, according to VA data.
Trauma-Focused Therapies: The Core of PTSD Treatment
Trauma-focused psychotherapies such as Cognitive Behavioral Therapy (CBT) and Eye Movement Desensitization and Reprocessing (EMDR) remain the gold standard. According to research from the University of Texas at Dallas, these therapies have:
- An 85% response rate (notable symptom improvement)
- Around 40% achieve full remission
- 20% dropout rates, indicating challenges in sustaining engagement
These therapies work by processing traumatic memories and reshaping cognitive responses to triggers, enabling individuals to regain control over anxiety and hypervigilance that PTSD produces.
Prolonged Exposure Therapy and Cognitive Processing Therapy, often used by the VA, are structured forms of trauma-focused therapy that involve gradual, safe exposure to trauma memories and triggers, resulting in 53% full remission in some veteran-focused studies.
Medications: Supporting Recovery
While medications alone rarely resolve PTSD fully, Selective Serotonin Reuptake Inhibitors (SSRIs) and Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs) remain important tools for symptom management, especially when integrated into structured treatment plans that include psychotherapy.
These medications help regulate mood, reduce hyperarousal, and dampen intrusive thoughts, providing a stabilizing effect that can make it easier for individuals to engage in trauma-focused therapies.
According to VA clinical data, about 62% of patients using medications show measurable symptom improvement, including reductions in anxiety, depression, and sleep disturbances. Among veterans, 42% reach remission when using medication-based approaches in conjunction with therapy, underscoring the importance of a multi-layered treatment strategy.
It’s important to note that side effects, patient adherence, and the right medication match can influence outcomes, so regular monitoring and communication with healthcare providers are critical to maximizing the benefits of pharmacotherapy in PTSD treatment.
Advanced and Emerging Therapies

Vagus Nerve Stimulation (VNS)
Vagus nerve stimulation (VNS) is emerging as a promising adjunctive therapy for PTSD, particularly for individuals who have not fully responded to traditional treatments. A 2025 study from UT Dallas found that VNS combined with CBT resulted in an 85% response rate and 40% remission, with participants experiencing significant reductions in hyperarousal, anxiety, and avoidance symptoms.
VNS operates by modulating neural circuits linked to fear, stress response, and emotional regulation, providing a non-drug-based alternative that can enhance the brain’s capacity to process traumatic memories and regulate mood.
According to UT Dallas researchers, VNS could become a viable option in integrated PTSD treatment programs, especially for veterans seeking drug-free adjuncts to therapy.
If you’re concerned about your mental health or experiencing persistent stress and avoidance symptoms, you can take a free personal mental health and personality assessment at https://breeze-wellbeing.com/borderline-personality-disorder/
This can help you understand your current state and guide you on whether it’s time to seek structured PTSD care.
AI-Enhanced Neurofeedback (Prism)
AI-based neurofeedback systems like Prism are rapidly gaining attention in the PTSD treatment landscape. These systems utilize real-time brainwave monitoring and feedback loops to train individuals to re-pattern maladaptive neural responses to stress and trauma cues.
Coverage of this technology, 67% of participants in clinical trials reported significant symptom improvement, while 33% achieved full remission, demonstrating the potential of AI-enhanced neurofeedback in reshaping how PTSD is treated.
Key benefits of Prism and similar systems include:
- Non-invasive, drug-free intervention
- Potential for home-based or clinic-based use
- Personalized therapy adjustments using AI analysis of neural patterns
- Higher engagement rates among individuals hesitant about traditional therapy
By providing individuals with direct control over their brain’s stress responses, Prism could become a powerful tool for those seeking autonomy in their recovery journey.
Virtual Reality Exposure Therapy (VRET)
Virtual Reality Exposure Therapy (VRET) is now validated and supported by the Department of Defense as an effective method for addressing PTSD, particularly among veterans.
VRET uses immersive, controlled virtual environments to simulate trauma-related scenarios safely, allowing individuals to confront and process traumatic memories under the guidance of a clinician.
- Greater flexibility in session structure
- Increased patient engagement through interactive environments
- Controlled pacing of exposure tailored to patient tolerance
For many patients, VRET offers a safe, structured path to confronting and integrating traumatic experiences while reducing the overwhelming anxiety often triggered by direct exposure in real-world environments.
Psychedelic-Assisted Therapies
@60minutes In one study, 45% of vets with PTSD who did MDMA-assisted therapy at the VA went into full remission, says Dr. Elnahal. #60minutes #veterans #psychedelic #ptsd ♬ original sound – 60 Minutes
Psychedelic-assisted therapies, including MDMA- and psilocybin-assisted psychotherapy, are progressing toward FDA approval and are increasingly viewed as potential breakthrough treatments for PTSD.
According to MAPS and VA-funded studies, these therapies, when combined with guided psychotherapy sessions, can produce significant reductions in PTSD symptoms and may offer pathways to long-term remission.
In these treatments:
- MDMA facilitates emotional openness and reduces fear during trauma processing.
- Psilocybin can promote perspective shifts, emotional breakthroughs, and enhanced connectivity in the brain.
States like Colorado have legalized psilocybin therapy under medical oversight, while bipartisan support in Congress is growing to expand veteran access to psychedelic treatments, as reported by PubMed.
Although these therapies are still under regulatory review, their potential to transform treatment-resistant PTSD care is notable, with many patients reporting profound improvements in symptoms and quality of life.
Market Trends in PTSD Treatment
The PTSD treatment market in the U.S. was valued at $1.03 billion in 2024 and is projected to grow to $1.57 billion by 2034, reflecting a 4.3% compound annual growth rate (CAGR) according to Precedence Research.
Driving factors behind this growth include
- Rising demand for accessible, effective mental health care
- Integration of AI, telehealth, and VR technologies into treatment models
- Policy momentum supporting innovative and advanced therapies
- Persistent and growing need for PTSD care among veterans and civilians alike
This growth reflects not only the increasing societal recognition of PTSD’s impacts but also shifting treatment preferences toward integrative, technology-enhanced, and personalized care.
Barriers to Access

Challenges include
- High treatment costs and inconsistent insurance coverage for advanced therapies
- Provider shortages, particularly in rural and underserved areas
- Stigma surrounding mental health and PT, many from seeking help
- Complex navigation of treatment options, leading to confusion about where to start and what treatments are available
According to Mission Roll Call and related advocacy organizations, over 40% of Americans with mental illnesses, including PTSD, remain untreated due to these barriers.
Efforts are underway to address these challenges:
- Expansion of telehealth to improve rural access
- Policy advocacy for insurance coverage of advanced treatments
- Educational campaigns to reduce stigma and encourage early intervention
- Pilot programs in VA systems to increase the availability of therapies like VRET, Prism, and psychedelic-assisted treatments for veterans
Methodology
This article was developed using a systematic review of current 2025 PTSD treatment data. We synthesized quantitative findings on treatment modalities, including trauma-focused therapies, pharmacotherapy, neuromodulation, and psychedelic-assisted interventions, emphasizing response and remission rates.
Structured tables were incorporated to facilitate comparative analysis of treatment efficacy across modalities. Market projections were integrated using current industry data from Precedence Research to contextualize economic trends in PTSD treatment.
Accessibility barriers were examined using policy and advocacy reports, including Mission Roll Call data, to assess gaps in care delivery. The article was crafted to maintain clarity, academic rigor, and practical relevance, supporting informed decision-making for healthcare professionals and stakeholders in PTSD care.
Conclusion
Mental health matters. For those suffering from PTSD, there is a new device that can help with treatment. Read more about how #TechnionAlumni are helping treat PTSD.https://t.co/NUCLU1qsd5 #Technion #TechnionImpact
— American Technion Society (@TechnionUSA) March 6, 2024
PTSD treatment in America in 2025 works, but results depend heavily on consistent, structured care and access to the right therapies. Trauma-focused therapies like CBT and EMDR remain the foundation, providing real symptom relief and remission for many.
Medications can ease the intensity of symptoms, especially when paired with therapy, helping people regain daily function and sleep.
Advanced treatments like vagus nerve stimulation, AI neurofeedback systems like Prism, and virtual reality exposure therapy are proving effective for patients who do not fully respond to standard care, with measurable improvements backed by recent clinical data.
Psychedelic-assisted therapies, including MDMA and psilocybin, are moving closer to regulated use and show strong early outcomes in reducing PTSD symptoms.
Still, barriers like high costs, lack of providers, and stigma prevent over 40% of Americans with PTSD from getting treatment. This is not just a policy issue but a practical gap: many who need care the most cannot get it.
The market for PTSD treatment is growing, reflecting the demand, but growth alone does not guarantee equitable access. For real impact, efforts must focus on reducing costs, expanding coverage for advanced therapies, and supporting community-based and telehealth models that bring these effective treatments to those who need them.
In short, PTSD is treatable, and treatments are improving. The next step is ensuring these treatments are available and sustainable for everyone who needs them in America.