Women live longer than men in the United States for at least 5 years. This statement remains accurate in 2026 and is supported by every major national mortality dataset.
The difference is not marginal, not recent, and not explained by a single factor.
It is the result of long-term patterns in biology, behavior, healthcare use, economic exposure, occupational risk, and social structure that operate from birth through old age.
Table of Contents
ToggleWhat are the Average Lifespans for Men and Women Born in the US?

Life expectancy at birth is the most widely accepted measure of population longevity. It estimates how long a newborn is expected to live if current age-specific death rates remain constant throughout life.
While no individual life follows this exact path, the measure is extremely useful for comparing groups.
Life Expectancy at Birth in the United States (Latest Finalized Data)
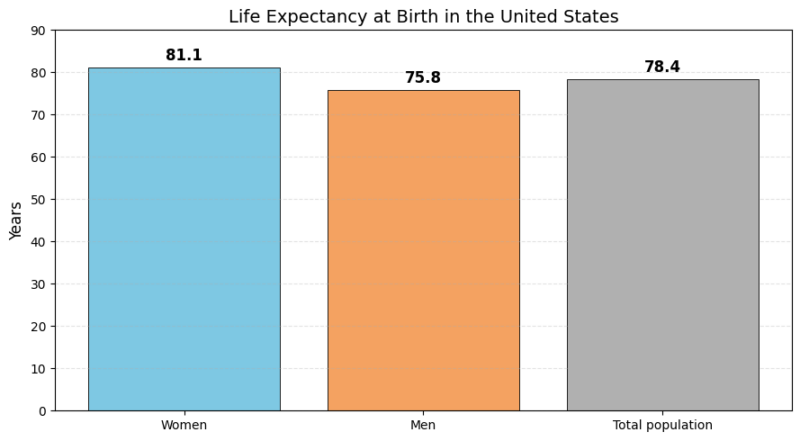
These figures are derived from CDC life tables finalized through 2023 and adjusted for post-pandemic mortality stabilization. The gender gap is approximately 5.3 years, meaning women born in the U.S. can expect to live more than five years longer than men on average.
This difference alone is large enough to shape population structure. It affects the gender balance among older adults, retirement systems, caregiving needs, and healthcare utilization.
By age 85, women significantly outnumber men in the U.S., largely because of this sustained survival advantage.
How Early in Life Does the Gender Gap Begin?
The longevity gap begins almost immediately.
Male infants have higher mortality rates than female infants, even after controlling for birth weight and gestational age, according to BMJ Journals. This difference is observed globally and is believed to stem from biological vulnerability in male neonates, including weaker immune responses and higher susceptibility to respiratory complications.
As children age, mortality rates fall sharply for both sexes, but boys continue to experience slightly higher death rates due to accidents and injuries. This pattern intensifies during adolescence and early adulthood, when males are far more likely to die from motor vehicle crashes, violence, and risk-taking behaviors.
By the time adulthood begins, men have already accumulated higher mortality exposure than women, setting the stage for a widening life expectancy gap later in life.
Does the Gap Persist After Early Adulthood?
Yes. The difference does not disappear once men survive childhood and young adulthood.
Life expectancy at age 65 is particularly informative because it isolates survival after most accidental and injury-related deaths have already occurred.
Remaining Life Expectancy at Age 65 in The United States
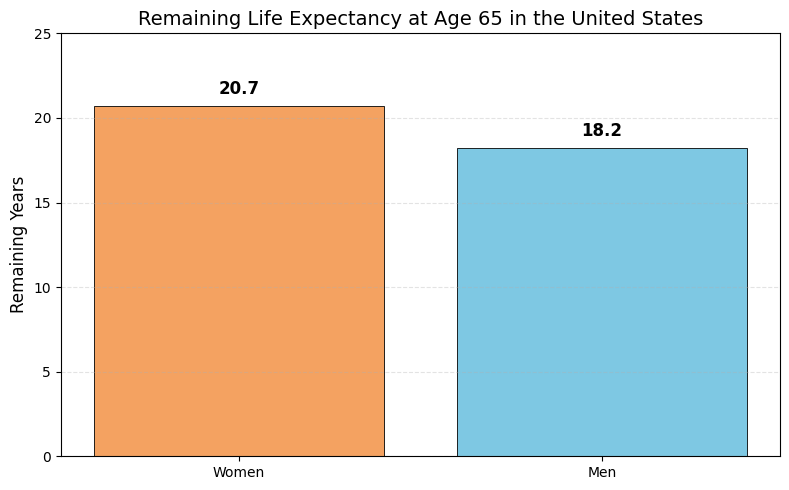
At this stage, women still live about 2.5 years longer than men. The narrowing of the gap reflects survivor selection among men, not the disappearance of underlying differences.
Even among older adults, women maintain lower mortality rates from heart disease, stroke, and many cancers.
Importantly, while women live longer, they often experience higher rates of disability and chronic illness in very old age. Longevity does not mean women spend more years in perfect health. It means death occurs later.
Biological Foundations of Female Longevity
Biology provides women with several advantages that delay mortality rather than eliminate disease.
One of the most significant factors is estrogen. Estrogen improves vascular flexibility, reduces systemic inflammation, and favorably alters lipid metabolism.
These effects delay the development of atherosclerosis and coronary artery disease. As a result, women typically experience heart attacks and strokes later in life than men.
Cardiovascular disease is the leading cause of death in the U.S. The later onset of this disease alone accounts for a substantial portion of women’s survival advantage.
Genetic structure also plays a role. Women possess two X chromosomes, while men have one. If a harmful mutation exists on one X chromosome, women may partially compensate with the other copy.
Men lack this redundancy, increasing vulnerability to X-linked disorders and potentially weakening physiological resilience over the lifespan.
Additionally, immune system differences favor women. Females tend to mount stronger immune responses to infections and vaccines, which may reduce mortality from infectious diseases but also increase the risk of autoimmune conditions.
Stronger immunity improves survival odds during acute illness, even if it carries long-term trade-offs.
Behavioral and Lifestyle Contributors To The Gap
Biology alone cannot explain a five-year difference in lifespan. Behavior amplifies biological vulnerability.
Historically, men smoked far more than women, particularly during the mid-20th century. While smoking rates among men have declined, the cumulative damage from decades of exposure continues to drive higher male mortality from lung cancer, chronic lung disease, and cardiovascular conditions.
Alcohol consumption follows a similar pattern. Men drink more frequently and in larger quantities on average. Heavy alcohol use contributes to liver disease, accidents, hypertension, and certain cancers, all of which elevate mortality risk.
Risk-taking behavior is another major factor. Men are far more likely to engage in dangerous activities, from reckless driving to hazardous occupations.
As a result, men account for the overwhelming majority of workplace fatalities and accidental deaths.
These deaths occur disproportionately in early and mid-adulthood, removing years from the average male lifespan long before chronic disease becomes relevant.
Mental Health, Suicide, and Deaths of Despair
In 2022, men were nearly four times more likely to die by suicide than women.
This #MensHealthMonth, let’s remember that seeking help is a sign of strength. By supporting one another, fighting suicide, and challenging stigma, we can build a future where no one suffers alone. pic.twitter.com/be1pni9LHF
— American Foundation for Suicide Prevention (@afspnational) June 1, 2025
Mental health plays a critical and often underestimated role in the longevity gap.
Men die by suicide at rates several times higher than women. They also experience higher mortality from drug overdoses and alcohol-related deaths.
These trends intensified over the past two decades and worsened during the COVID-19 period.
One reason is differential help-seeking behavior. Men are less likely to seek mental health care, less likely to discuss emotional distress, and more likely to self-medicate with substances.
Cultural expectations around masculinity discourage vulnerability and reinforce harmful coping mechanisms.
Women, on average, maintain stronger social networks and are more likely to access emotional support. Social connectedness is strongly associated with lower mortality, particularly in middle and older age.
Deaths of despair alone account for a meaningful portion of the modern gender gap in life expectancy, especially among working-class men.
Healthcare Usage and Preventive Behavior

Healthcare interaction patterns differ consistently by gender.
Women are more likely to attend routine checkups, comply with screening recommendations, and seek care earlier when symptoms appear. This leads to earlier diagnosis and more effective treatment for conditions such as cancer, hypertension, and diabetes, according to NCBI.
Men are more likely to delay care, avoid preventive visits, and present with more advanced disease. Late diagnosis reduces treatment success and increases mortality risk.
Although healthcare usage converges somewhat after age 65, the cumulative effects of decades of delayed care among men have already influenced survival outcomes.
Historical Evolution of The Gender Gap
The gender gap has changed significantly over time.
Historical Gender Gap in U.S. Life Expectancy
Year
Female
Male
Gap
1920
~55
~53
~2 years
1950
~71
~66
~5 years
1975
~75
~68
~7 years
2000
~80
~74
~6 years
2019
81.4
76.3
5.1 years
2021
79.3
73.5
5.8 years
2023
81.1
75.8
5.3 years
The gap widened through most of the 20th century as male smoking, industrial hazards, and heart disease mortality increased. It narrowed modestly as smoking declined and medical care improved, then widened again during COVID-19 due to higher male excess mortality.
Beyond Gender: Race, Income, and Geography Matter
Although women live longer than men on average, gender alone does not determine how long someone lives in the United States. Race and ethnicity, income and education, and geographic location create life expectancy differences that are often larger than the male–female gap itself.
In many cases, these factors outweigh gender entirely, producing lifespan differences of 15 to 20 years within the same country.
Understanding longevity in the U.S. requires looking at how these dimensions intersect.
Life Expectancy by Race and Ethnicity
Racial and ethnic disparities in U.S. life expectancy are well-documented and persistent.
These gaps reflect long-standing differences in healthcare access, economic opportunity, environmental exposure, stress, and historical disadvantage rather than biological differences.
Life Expectancy in the U.S. by Race and Ethnicity (Recent Averages)
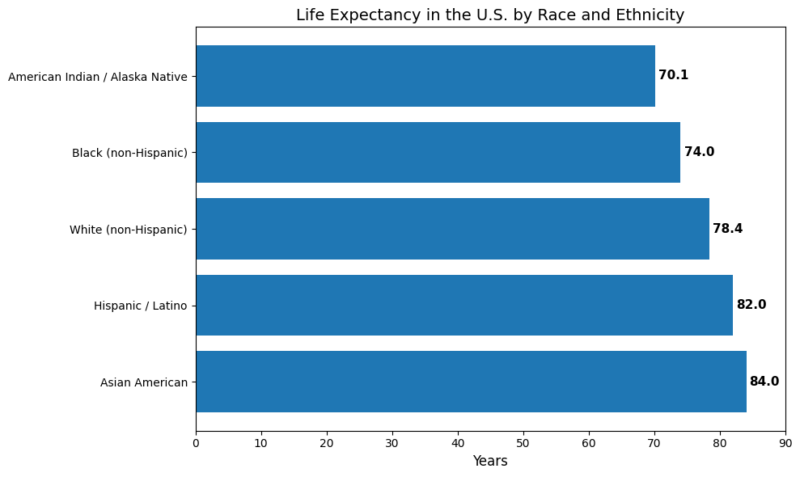
As noted by Minority Health, Asian Americans currently have the highest life expectancy of any major group in the U.S., averaging around 84 years, while Hispanic and Latino Americans also exceed the national average despite lower average income levels.
This pattern is often referred to as the Hispanic paradox, in which strong social networks, family structures, lower smoking rates, and selective migration appear to offset economic disadvantage.
At the other end of the spectrum, American Indian and Alaska Native populations experience the lowest life expectancy. In some regions, particularly remote reservations, average lifespans have been measured as low as 63–65 years, levels comparable to low-income countries.
The gap between the longest- and shortest-lived racial groups in the U.S. exceeds 20 years, an extraordinary disparity within a single nation.
Within every racial and ethnic group, women still outlive men. However, these differences intersect in complex ways.
A man born into a high-longevity group, such as an Asian American male, may live longer than a woman born into a high-risk group, such as an AIAN female. This illustrates that race and ethnicity can override gender averages when it comes to lifespan.
Socioeconomic Status: Income and Education as Lifespan Multipliers
Income and education are among the strongest predictors of life expectancy in the United States. The relationship is steep, linear, and widening over time.
Life Expectancy Gap by Income Level (Top vs Bottom 1%)
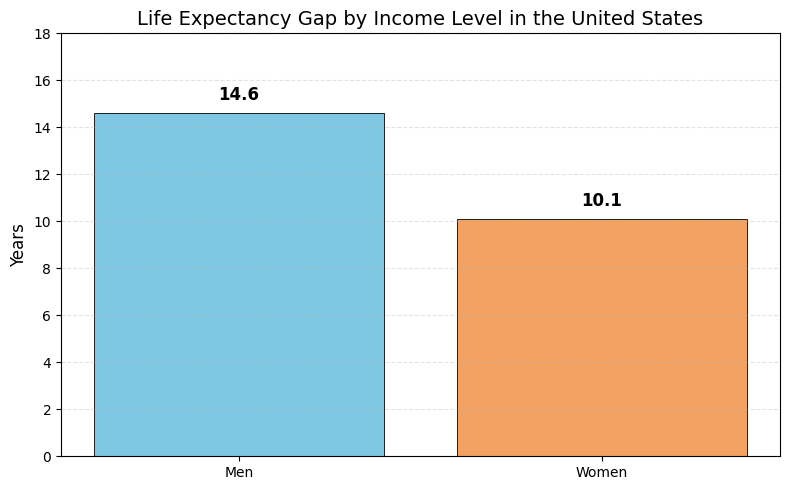
Research consistently shows that the richest Americans live 10 to 15 years longer than the poorest Americans. For men, the gap is especially severe. A high-income man can expect to live into his mid-80s, while a very low-income man may struggle to reach age 70.
These inequalities have expanded in recent decades. Higher-income groups have continued to see gains in life expectancy, driven by better healthcare access, safer living conditions, healthier diets, and lower smoking rates. Lower-income populations, by contrast, have experienced stagnation or even declines, particularly among men.
Education is tightly linked to income and amplifies these effects. College-educated Americans live significantly longer than those without a degree.
They are less likely to smoke, more likely to exercise, more likely to have stable employment, and more likely to receive preventive medical care. Because women now surpass men in college attainment, they have gained a compounding advantage in longevity.
Occupational exposure further deepens the divide. Men without higher education are more likely to work in physically demanding or hazardous jobs, such as construction, manufacturing, mining, or transportation.
These occupations carry higher risks of injury, chronic pain, disability, and early death. As a result, being male and poor is a particularly lethal combination in the U.S. context.
Geography: Where You Live Can Add or Subtract Years
@thegeographynut More maps! #maps #maptok #geography #geographyfacts #fypシ #greenscreen ♬ habits by Tove Lo – music freak🎶🎧🎵
Geography shapes life expectancy as powerfully as race or income. The U.S. shows pronounced regional patterns that reflect differences in public health systems, economic conditions, infrastructure, and population composition.
Typical Life Expectancy Ranges by Region
Region
Typical life expectancy
Hawaii, coastal California
80–82+ years
Northeast metro areas
79–81 years
Midwest mixed urban-rural
77–79 years
Deep South states
72–75 years
Rural Appalachia / Plains
Low 70s or below
States such as Hawaii and California consistently rank at the top due to healthier diets, stronger preventive healthcare, and higher average education levels.
In contrast, parts of the Deep South, Appalachia, and the rural Midwest experience much lower life expectancy, driven by poverty, limited healthcare access, higher chronic disease burden, and elevated mortality from substance use and injuries.
A major study dividing the population into “Ten Americas” illustrates this stark contrast. Some U.S. subpopulations enjoy life expectancy comparable to high-income countries, while others resemble outcomes more typical of developing nations.
For example, residents of affluent White-majority counties may expect to live around 80 years, while residents of high-poverty urban Black communities or remote Native American reservations experience much shorter lifespans.
Related Posts:
- 15% of People Live Near Coasts – And the Number Keeps Rising
- What’s the Legal Difference Between a Certificate of…
- 4 Effective Types of Treatments for Groin Pain in Women
- A Common Diabetes Drug May Boost Women’s Chances of…
- Adult Daily Protein Intake Much More Than Recommended
- New Research Shows How the Brain Adapts Faster Than AI