Over 280 million people across the globe experience depression, while anxiety disorders impact more than 301 million, according to the World Health Organization.
Cognitive Behavioral Therapy (CBT) has emerged as one of the most evidence-based approaches for treating these conditions, offering effective results with minimal side effects.
With success rates reported between 50 and 75 percent, CBT provides meaningful improvement for many individuals struggling with mental health challenges.
With the CBT success rate in mind, we believe taking a look at all other relevant statistics regarding CBT is worth it.
What Does CBT Stand for Exactly?
CBT, or Cognitive Behavioral Therapy, is one of the most widely researched and applied forms of psychotherapy in the modern era.
It grew out of Dr. Aaron Beck’s pioneering work in the 1960s, which emphasized how distorted thoughts influence emotions and actions.
CBT is generally short-term and goal-focused, making it accessible and manageable for many patients.
Treatment aims to help individuals recognize unhelpful thinking patterns and replace them with healthier ways of interpreting and responding to life events.
Instead of spending years revisiting past experiences, CBT emphasizes present challenges and practical coping strategies that can be applied immediately.
Sessions often involve homework assignments, structured exercises, and skill-building tasks.
Patients are encouraged to practice techniques outside of therapy sessions, reinforcing positive changes and promoting self-reliance.
Applications extend across a wide range of conditions:
Long-Term Impact & Real-World Effectiveness

Long-term studies confirm its ability to deliver lasting results, while real-world applications such as online and mobile-based therapy make it widely accessible across populations.
Remission Durability
Depression outcomes show lasting remission rates that persist long after treatment ends.
Immediate post-treatment remission reaches 61.38 percent, climbing to 75 percent at six months.
Even after more than four years, 63.64 percent of patients maintain remission, reflecting long-term stability.
Routine Care Performance
Internet-based CBT (iCBT) offers an accessible alternative to in-person therapy.
To explore your options, you can find a therapist with Therapy Den, a mental health platform featuring professionals from a wide range of backgrounds and specialties.
With an effect size of g = 0.38, its results are comparable to face-to-face sessions.
Mobile apps provide effect sizes ranging from d = 0.34 to 0.56, though they often face higher dropout rates due to limited patient engagement and reduced accountability.
Global Evidence
The effectiveness of CBT is not restricted to Western countries.
Research in non-Western populations shows effect sizes of g = 1.10 for anxiety and g = 1.41 for depression.
In low- and middle-income countries, effect sizes range from d = 0.72 to 2.62, demonstrating extraordinary applicability across cultural and economic contexts.
Factors Influencing CBT Success
The effectiveness of CBT depends on a combination of therapist, patient, and environmental factors.
Research pointed out several variables that significantly affect outcomes:
Factor
Impact Level
Effect Size
Therapist expertise
High
g = 0.55–0.80
Patient engagement
Very high
g = 0.70–0.90
Symptom severity
Moderate
g = 0.40–0.60
Comorbid conditions
Moderate–high
g = 0.30–0.50
Social support
Moderate
g = 0.35–0.55
Patient engagement plays the largest role in determining treatment success.
When individuals are active participants, outcomes improve dramatically.
Skilled therapists further boost results by tailoring approaches to patient needs.
Severity of symptoms, presence of additional conditions, and social support networks also influence effectiveness.
General CBT Success Rates (All Ages)

The effectiveness of CBT has been confirmed across hundreds of studies and tens of thousands of participants.
Results demonstrate that this therapy consistently produces measurable improvements in mental health outcomes, making it a trusted option for both clinicians and patients.
Efficacy and Effect Sizes
Meta-analyses covering more than 409 trials and over 52,000 patients highlight the power of CBT.
When compared with control groups, average effect sizes reach g = 0.79, which falls into the moderate-to-large range.
Outcomes remain strong over time, with g = 0.74 at six to nine months and g = 0.49 at ten to twelve months, demonstrating the durability of results.
Response and Remission Rates
Response rates average 42 percent for patients undergoing CBT compared to 19 percent in control conditions.
For those diagnosed with depression specifically, nearly half achieve a positive response.
Remission rates also tell a compelling story, with 36 percent in CBT groups compared to only 15 percent in controls.
Numbers Needed to Treat (NNT) further emphasize clinical value, at 4.7 for response and 3.6 for remission.
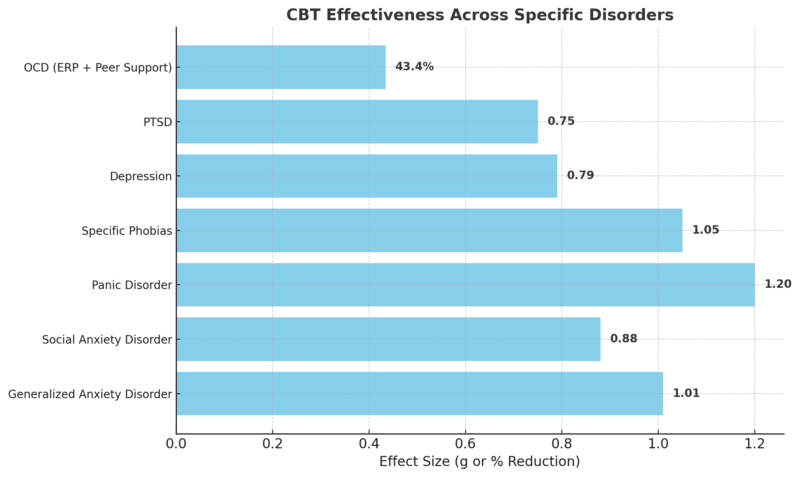
Specific Disorders Effectiveness
CBT demonstrates measurable effectiveness across multiple conditions:
Satisfaction, Adherence & Dropouts
Patient satisfaction rates are consistently high, with 70 percent reporting a positive experience.
Around 60 percent show significant improvement during treatment.
Dropout rates remain relatively low, averaging 20 percent across conditions.
OCD treatment can present challenges, with nonadherence ranging between 31 and 65 percent.
Peer-supported exposure therapy shows promise, with symptom reduction averaging 43.4 percent.
CBT for Older Adults – Enhanced CBT-OA
As populations age, tailoring therapy to meet the needs of seniors has become increasingly important.
Standard CBT methods may not always be optimal for older adults who face unique challenges, including frailty, sensory limitations, and slower cognitive processing.
Enhanced CBT for Older Adults (CBT-OA) addresses these needs through practical adjustments that make therapy more accessible and engaging.
Why Modify CBT for Seniors?

Older adults often process information differently and may require adaptations in how therapy is delivered.
Larger fonts, simplified writing tasks, mid-week coaching calls, mnemonic aids, and frequent repetition of core concepts help increase retention and engagement.
These modifications acknowledge the learning needs of seniors and respect their expectations for therapy.
Study Overview
One clinical study examined 49 older adults, with 40 completing the program.
Participants were divided into “young-old” under age 78 and “old-old” over age 78.
Treatment spanned seven to nine weeks, with group sessions held once a week for two hours.
Results
Outcomes showed meaningful benefits for older participants:
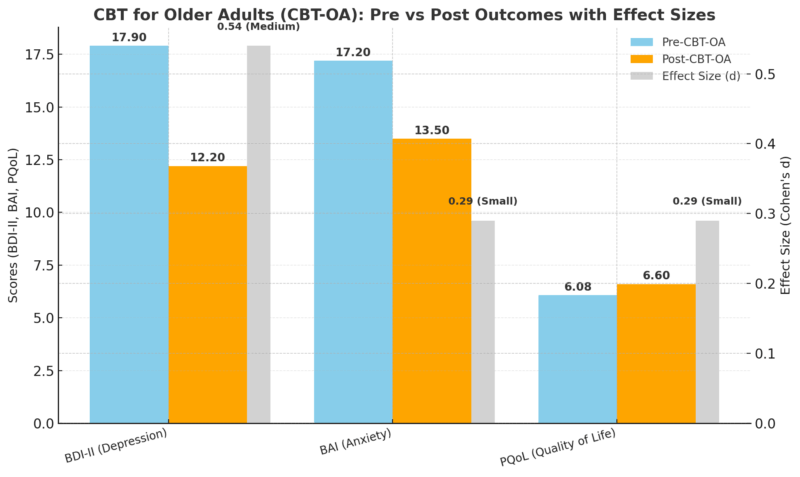
Young-old participants achieved stronger gains in both depression and anxiety compared to old-old individuals.
Results suggest that tailoring CBT to the needs of seniors significantly enhances outcomes, especially among younger elderly patients.
Limitations
Research on CBT has produced impressive results, yet certain methodological and practical challenges must be acknowledged.
Limitations in design, measurement, and population-specific outcomes highlight areas where findings should be interpreted with caution and where improvements in research design are needed.
Research Design Challenges
Many CBT studies rely on observational methods rather than randomized controlled trials.
It introduces the risk of bias, as outcomes may reflect influences unrelated to therapy itself.
Participants may change behavior simply because they know they are being observed, a phenomenon sometimes called the Hawthorne effect.
Regression to the mean can occur, where extreme symptoms naturally lessen over time regardless of treatment.
Measurement Limitations

CBT effectiveness is often assessed using self-reported surveys and questionnaires. While useful, these methods are prone to exaggeration or selective recall.
Patients may unintentionally overstate progress to please therapists or to align with perceived expectations.
Standardized quality-of-life tools might not capture subtle emotional or psychological changes that patients genuinely experience.
Population-Specific Concerns
Older adults present unique challenges when evaluating therapy outcomes. Frailty, physical health limitations, and slower cognitive processing may blunt measurable results.
Some may find it difficult to complete written assignments or participate fully in structured tasks.
Existing assessment tools may not reflect meaningful improvements, particularly in social connectedness or daily coping ability.
Implications for Future Research
Acknowledging these limitations does not diminish the value of CBT but highlights the need for ongoing refinement.
Broader use of objective biological markers alongside self-reports could strengthen accuracy.
Longitudinal studies tracking patient progress over decades would provide a clearer view of long-term benefits.
Designing tailored assessment tools for older adults and specific populations would offer more precise measurements of progress.
Recognizing and addressing these gaps ensures that CBT research continues to evolve, leading to even stronger and more reliable evidence of effectiveness.
Summary
Most viewed in the last 7 days from @JAMAPsych:
Cognitive behavior therapy (CBT) is generally effective for treating major depression, anxiety disorders, PTSD, OCD, and eating disorders. https://t.co/C8yQsmV0UT pic.twitter.com/8KtkkSziGk
— JAMA Psychiatry (@JAMAPsych) April 27, 2025
CBT consistently achieves success rates between 50 and 75 percent across both anxiety and depression.
Results remain significant across age groups, clinical settings, and global populations.
Enhanced versions such as CBT-OA show promise in adapting treatment for older adults, with younger seniors responding particularly well.
Cost-effectiveness, tolerability, and strong long-term remission outcomes confirm CBT as one of the most effective psychological therapies available today.
Related Posts:
- How Common Is Postpartum Depression? U.S. Statistics…
- Teen Depression Statistics in the US - A Closer Look…
- US Software Jobs Are Set to Grow 15 Percent by 2034…
- 4 Effective Types of Treatments for Groin Pain in Women
- One Weight Loss Strategy Is Far More Effective Than…
- US vs Europe Healthcare in 2025 - Costs, Quality of…