Postpartum depression (PPD) is a type of depression that happens after childbirth. It affects many new mothers, making them feel very sad, tired, anxious, or unable to connect with their baby. Unlike the “baby blues,” which go away in a few days, PPD can last for months if untreated.
Doctors believe it happens because of changes in hormones, stress, and lack of support. Many women do not know they have PPD or are afraid to talk about it, so they do not get help.
Many apps, like Femia, help women track their pregnancy and fertility. These tools give support, but postpartum depression is still common. Knowing the risk factors and signs can help women get treatment sooner.
This article explains how common PPD is in the U.S., what raises the risk, and why early help is important.
Postpartum Depression: Definition, Prevalence, and Undiagnosed Cases
Women with PPD may struggle to bond with their baby, have trouble sleeping, or feel like they are not good mothers. Doctors believe hormonal changes, stress, and lack of support contribute to PPD.
PPD is very common. About 1 in 7 women experience postpartum depression in the first year after giving birth. Some studies suggest it may be even higher because many cases go unreported.
Each year, around 600,000 women in the U.S. are diagnosed with PPD. If women who had miscarriages or stillbirths are included, the number increases to 900,000 annually.
‘Finding peer support meant the world to me.’
Thank you to this mum for sharing your story: https://t.co/KqqZdQ7zsU
💜 If you have been affected by this story, need any support, or want to meet others affected by postpartum psychosis, get in touch: https://t.co/kpUFgZxAvg pic.twitter.com/bqNzIL25E3
— Action on Postpartum Psychosis (@ActionOnPP) January 13, 2025
Why Do So Many Cases Go Undiagnosed?
Many women with PPD do not seek help. About 50% of cases go undiagnosed. Some mothers feel ashamed or afraid of being judged. Others may not know they have PPD and think their feelings are normal.
Doctors may also miss the signs if they do not ask the right questions during checkups. Better screening, education, and support can help more women get the treatment they need.
Risk Factors for Postpartum Depression
Many factors can increase the chances of developing postpartum depression. Some are related to past mental health issues, while others are linked to physical changes, social struggles, or problems during pregnancy and childbirth.
Medical History and Mental Health
- Past Depression or Anxiety – Women who had depression or anxiety before pregnancy have a 30-35% higher risk of developing PPD.
- Previous Postpartum Depression – Mothers who had PPD before have a 10-50% chance of experiencing it again.
- Family History of Mental Illness – A history of depression or bipolar disorder in close family members increases the risk.
Hormonal and Physical Changes
- Hormone Shifts – Estrogen and progesterone drop suddenly after childbirth, which can trigger depression.
- Thyroid Issues – Some women develop thyroid problems after pregnancy, leading to mood swings and fatigue.
- Lack of Sleep – Caring for a newborn often leads to extreme tiredness, which can make PPD worse.
Social and Economic Challenges
- Lack of Support – Women who do not have emotional or practical help from family and friends are at higher risk.
- Financial Stress – Low-income mothers are 11 times more likely to develop PPD than those with financial stability.
- Teen Mothers – Young mothers under 25 have higher rates of postpartum depression.
Pregnancy and Birth Complications
- Difficult Pregnancy – High-risk pregnancies or long periods of bed rest can lead to increased stress and depression.
- Traumatic Birth – Emergencies like unplanned C-sections or complications during delivery raise the risk of PPD.
- Miscarriage or Stillbirth – Women who lose a baby are at an increased risk of postpartum depression.
Postpartum Depression by Race and Ethnicity

Postpartum depression (PPD) rates have risen significantly in the U.S. over the past decade. The condition affects women of all racial and ethnic backgrounds, but research shows differences in prevalence across groups.
Factors such as access to healthcare, economic conditions, and social support contribute to these disparities.
PPD Rates by Race and Ethnicity
A study released in the American Journal of Obstetrics and Gynecology analyzing over 442,000 births found that PPD rates more than doubled from 9.4% in 2010 to 19.3% in 2021.
- White: 13.5% in 2010 → 21.8% in 2021 (60% increase)
- Black: 9.2% in 2010 → 22.0% in 2021 (140% increase)
- Hispanic: 8.9% in 2010 → 18.8% in 2021 (110% increase)
- Asian/Pacific Islander: 3.6% in 2010 → 13.8% in 2021 (280% increase, the largest increase)
Why Are PPD Rates Increasing?
- More Awareness and Screening – Increased screening has helped identify more cases, but many still go undiagnosed.
- Economic and Social Pressures – Stress related to job loss, inflation, and lack of paid leave may contribute to rising rates.
- Health Disparities – Some racial groups have less access to mental health care, which can delay diagnosis and treatment.
Postpartum Depression in Fathers
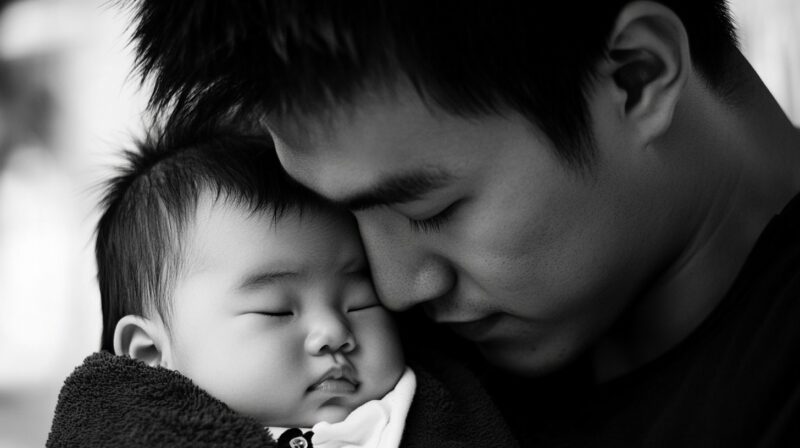
Postpartum depression is not just a problem for mothers. Fathers and adoptive parents can also experience depression after welcoming a new child. Lack of sleep, stress, and major life changes can lead to emotional struggles in both biological and non-biological parents.
Postpartum Depression in Fathers
- 10% of new fathers develop postpartum depression.
- If a mother has PPD, 50% of their partners also develop depression.
- Men often experience irritability, withdrawal, and anger instead of sadness.
It Also Affects Adoptive Parents
Adoptive parents can experience a condition similar to postpartum depression, known as post-adoption depression syndrome (PADS). This condition leads to symptoms such as anxiety, fatigue, changes in appetite, feelings of hopelessness, concentration problems, and, in severe cases, suicidal thoughts.
Studies report that 10% to 32% of adoptive parents experience post-adoption depression. A study from Purdue University found that while 71% of adoptive parents showed no or low depression symptoms, 6.2% experienced clinically significant levels of depression.
How Breastfeeding Affects Postpartum Depression

Breastfeeding has been linked to a lower risk of postpartum depression. The act of nursing releases oxytocin, a hormone that promotes relaxation and bonding between mother and baby. However, difficulties with breastfeeding can also contribute to stress and emotional struggles.
Benefits of Breastfeeding for Mental Health
- Lower Risk of PPD – Women who breastfeed tend to have lower rates of postpartum depression.
- Hormonal Support – Oxytocin and prolactin help improve mood and reduce stress.
- Stronger Mother-Baby Bond – Breastfeeding encourages physical closeness, which can help with emotional connection.
When Breastfeeding Becomes a Stressor
- Latching Issues – If a baby has trouble latching, it can lead to frustration and self-doubt for the mother.
- Pain or Low Supply – Some women struggle with pain or low milk production, making breastfeeding difficult.
- Pressure and Guilt – Mothers who cannot or choose not to breastfeed may feel judged, increasing feelings of guilt or sadness.
FAQs
Last Words
Postpartum depression is common, serious, and treatable. Many mothers struggle in silence, but help is available. Early screening, support from loved ones, and proper treatment can make a huge difference.
If you or someone you know is experiencing symptoms, reach out to a doctor or mental health professional. No one should face postpartum depression alone.
Related Posts:
- Anxiety and Depression Statistics - CBT Effective…
- Teen Depression Statistics in the US - A Closer Look…
- Your DNA Already Knows If You’ll Get Depression, New…
- Single Dose Of DMT Shows Rapid Relief From Major…
- Rising Dementia Risk and Its Burden on the United…
- Mental Health Trends Among Veterans – PTSD and…