Back pain does not begin with an accident or an aging joint. It often starts with daily habits, long hours of sitting, poor posture, or stress that settles deep into the lower back. People carry pain across their workdays, store it in their spines through sleepless nights, and treat it as a condition they must endure rather than treat.
Over time, it grows into something larger, disrupting jobs, altering lifestyles, and costing more than most realize.
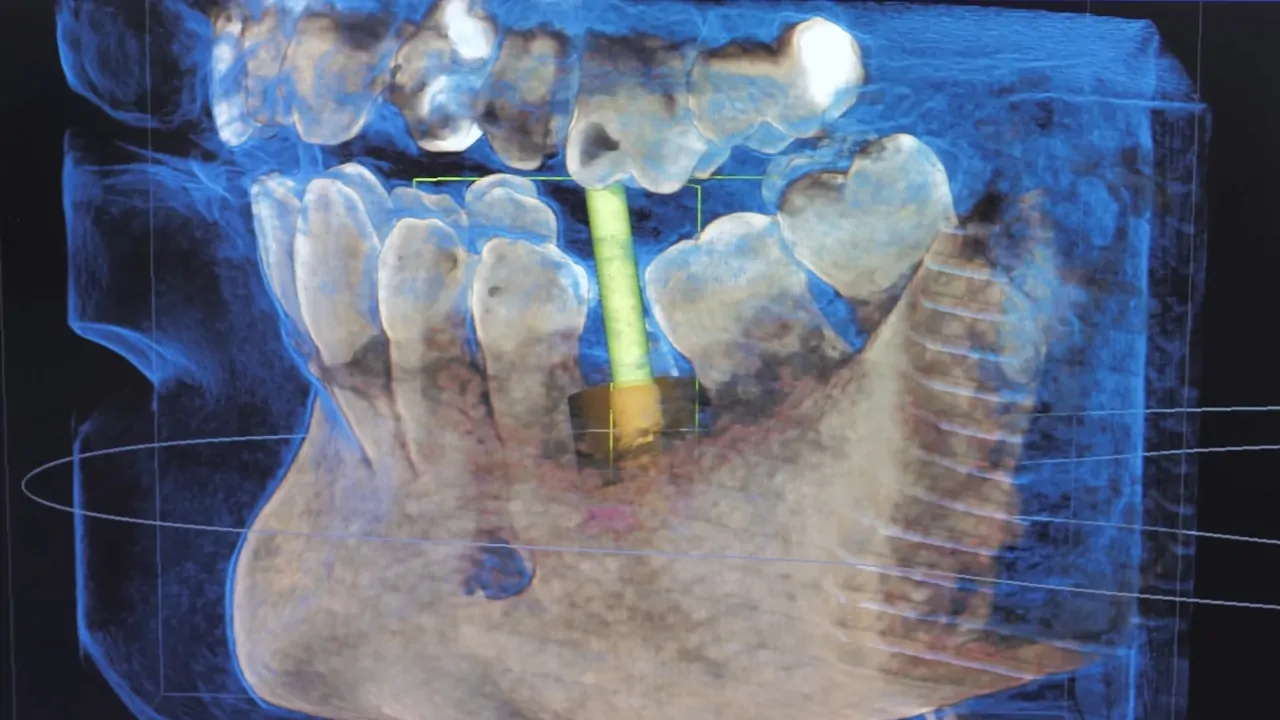
Surgery is not always the first or the final step. In fact, many cases show little improvement even after invasive procedures. Still, there are advanced solutions.
Premia Spine, for example, offers motion-preserving implants for certain lumbar conditions, especially when traditional fusion may not be ideal. At the same time, no product or procedure can reverse damage tied to years of poor movement or deeply rooted causes. Before any treatment begins, clear knowledge of the facts must come first.
The following report exposes the most alarming statistics about back pain in the U.S.
Table of Contents
Toggle1. Up to 80 Percent of Americans Will Experience Back Pain in Their Lifetime
Did you know more than 80% of Americans will experience low back pain at some point in their lives? Find out what you can do to help ease your back problems. https://t.co/gkCuI6hp8D pic.twitter.com/VwxtGQ92Pu
— WebMD (@WebMD) August 31, 2024
Back pain affects as many as 4 out of 5 people in the U.S. That rate places it among the most common health complaints, rivaling colds and seasonal flu in frequency.
The issue cuts across every demographic—young, old, active, sedentary. The underlying causes range from strained muscles to spinal degeneration. Many never trace the pain to a specific injury. It develops over time and stays.
Doctors see it not as a rare condition but as a routine part of adult life. Anyone can become part of the statistic without realizing it until the pain becomes severe enough to interrupt work, sleep, or mobility.
2. Lower Back Pain Is the Leading Cause of Work Disability
Back pain remains the number one cause of job-related disability in the U.S. It drives more workers out of jobs than any other musculoskeletal issue.
Employees miss critical days, and some leave the workforce altogether. The pain does not fade during office hours or warehouse shifts. It lingers, weakens focus, and lowers output.
- Workers with chronic back pain lose productivity equal to about 10 full workdays each year.
- Manual laborers, healthcare professionals, and office workers rank highest in disability reports due to back pain.
Workplace ergonomics only offers partial protection. Without proper care and prevention, minor strain evolves into long-term damage. The ripple effect shows up in wages, insurance claims, and lost careers.
3. 264 Million Workdays Are Lost Every Year to Back Pain
U.S. workers lose an estimated 264 million workdays each year because of back pain. That equals roughly two workdays per full-time employee.
This number does not reflect long hospital stays. Most missed days involve rest, recovery, or recurring episodes that flare up without warning. The economy absorbs the loss through slower output, temporary replacements, and rising healthcare premiums.
Breakdown by sector shows that:
- Healthcare, construction, and retail see the highest back pain-related absenteeism.
- Small businesses often carry the heaviest cost, with no backup for missing staff.
No pill, brace, or massage reverses the damage already done. Prevention through posture, lifting technique, and early intervention stands as the only shield against more days lost to a pain that never clocks out.
Here is where one overlooked group stands out: long-haul truck drivers. They spend long stretches seated, experience continuous road vibration, and often rest in restricted sleeping quarters.
Surveys show that 50-80 percent of truck drivers report chronic lower back pain, and researchers note that sleep surfaces inside truck cabins can influence symptom severity. Some industry reports mention that drivers use purpose-built truck mattresses, such as the Sleep Dog Mattress, to create more stable or supportive sleep conditions inside sleeper cabs.
Data from occupational health studies indicate that improved sleep environments can correlate with fewer pain flare-ups, reduced discomfort during long routes, and fewer missed workdays linked to back-related issues.
4. Back Pain Costs the U.S. Over 100 Billion Dollars Each Year
@banks601y Pain is profit, unfortunately. The back pain industry makes over $100 billion a year, and I’m just hoping spinal decompression keeps me off the surgery table. 🙏 Today, I had 10 lbs of traction on my neck and 8 on my back… and honestly, I felt like I was floating until the aftermath hit. 😩 You feel worse first, I can’t lie. The first time I did it. I was in bed for two days 🥴 Would you try this? 😵💫 #SpinalDecompression #BackPainRelief ♬ original sound – NFL
Back pain ranks among the most expensive medical conditions in the United States. The total annual cost exceeds 100 billion dollars, covering not only doctor visits and imaging but also lost productivity, missed wages, and disability claims.
- At least 50 billion dollars goes directly to healthcare spending.
- The remaining costs include workplace losses and reduced quality of life.
Health economists note that spending continues to rise as chronic pain cases grow. Many patients move between physical therapy, pain clinics, and surgical consults without long-term relief.
The financial burden stretches across public programs, private insurance, and household savings. Chronic back pain shapes not just health, but the entire economic landscape around it.
5. Nearly Half of All Americans Over 45 Report Back Pain
Age increases the likelihood of chronic pain. Among Americans aged 45 and older, nearly 46 percent experience back pain regularly. Even in younger adults, pain is common, but those in midlife and beyond report sharper and more frequent symptoms.
- About 28 percent of people in their 20s report recurring back pain.
- Among those 45 and older, nearly 1 in 2 lives with back pain as a regular condition.
- Women report slightly higher rates than men—41 percent vs. 37 percent.
6. Back Pain Is the Third Most Common Reason for Doctor Visits
After skin conditions and joint disorders, back pain holds the third spot as the most common reason people visit a doctor. Many arrive without a clear cause or injury, often after weeks or months of self-treatment.
What doctors encounter most:
- Persistent lower back pain with no trauma history
- Radiating pain into the hips or legs
- Stiffness that limits daily activity
Primary care physicians often refer patients to orthopedists, neurologists, or pain management specialists.
7. Most Back Pain Cases Are Not Linked to Serious Illness
The fear of a hidden disease drives many to the doctor. Yet the vast majority of back pain cases are mechanical in nature.
That means no tumor, no infection, no fracture—just muscle strain, joint pressure, or disc problems caused by movement patterns, posture, or age.
A closer look at the data:
- Over 90 percent of cases have no connection to cancer, infection, or spinal cord damage.
- Most are classified as nonspecific lower back pain.
Patients often expect scans or bloodwork to reveal a cause, but the pain rarely ties to a visible abnormality. The real issue usually comes down to weak core muscles, poor alignment, or repetitive stress. Solutions require active care—movement, therapy, posture correction—not just diagnostics.
8. Chronic Back Pain Rarely Stands Alone

People with long-term back pain often carry more than spinal discomfort. A CDC report found that nearly all adults with severe chronic back pain also suffer from at least one other chronic condition. The most common include arthritis, obesity, and depression.
Quick breakdown:
- Over 70 percent of those with back pain are overweight or obese.
- Nearly 50 percent have also been diagnosed with arthritis.
- Depression or anxiety appears in a significant portion of cases.
Back pain does not stay confined to the spine. It drains physical strength, fuels stress, and interrupts daily life. When pain persists, mental and physical health tend to decline together.
9. Opioids Are Still Used Widely—With Limited Long-Term Relief

Despite decades of concern and evolving guidelines, opioids remain one of the most prescribed treatments for back pain. Over half of long-term opioid users report back pain as their main condition. But outcomes remain mixed at best.
Research reveals the truth:
- Short-term pain relief peaks at about 30 percent.
- Long-term use shows no consistent functional improvement.
FAQs
Conclusion
Back pain does not follow a single pattern. It strikes without warning, lingers without answers, and spreads its cost across every part of life. The statistics shared here reveal more than numbers—they reflect millions of lives interrupted by discomfort that limits movement, drains energy, and reshapes health.
Treatment must begin with clarity. Not every case needs surgery. Not every case will respond to painkillers.
Sometimes the strongest step is early prevention through better movement, smarter care, and attention to lifestyle factors that slowly erode spinal strength. Options like physical therapy, posture correction, and targeted procedures such as those offered by Premia Spine provide alternatives where standard treatments fall short.
Related Posts:
- 10 Shocking Statistics About Heart Disease in 2025
- GLP-1 Is Not a Weight-Loss Shortcut - Doctors Push…
- Shocking Study Finds No Link Between COVID-19…
- 4 Effective Types of Treatments for Groin Pain in Women
- Experts Say This Ancient Gene Is Making Pain Feel Worse
- 7 Statistics That Highlight Age-Specific Trauma…