The U.S. is facing a growing shortage of nurses, both in the short and long term, with the gap in staffing seen at both the national and state levels.
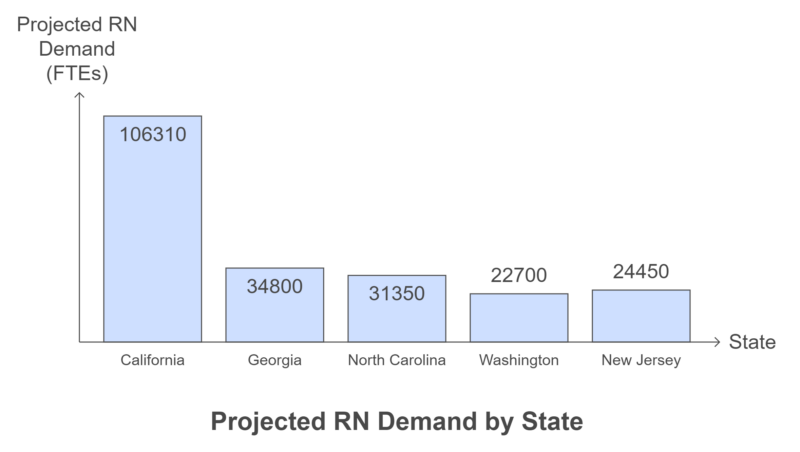
The most severe shortages in 2025 and on are projected in states like California, Georgia, and Washington, while North Dakota, South Dakota, and Utah have a surplus of nursing staff compared to demand, making them states with the highest demand for registered nurses.
This problem is especially pronounced in non-metropolitan and rural areas, where the shortage is more acute compared to urban, suburban, and metropolitan regions.
Nursing has long been seen more as a vocation than just a profession, yet it has grown into one of the most critical fields in healthcare.
According to the Bureau of Labor Statistics (BLS), nurses now make up over half of the health workforce in the U.S., playing a vital role in the entire healthcare system.
In fact, BLS data shows that 7 of the 20 fastest-growing jobs are nursing-related, and nursing is expected to lead the list of occupations with the highest increase in new jobs by 2032.
Table of Contents
ToggleWhich States Have the Highest Demand for Registered Nurses in 2024?

According to the Health Workforce Simulation Model (HWSM), that is designed to evaluate the future supply and demand of the nursing workforce. While the projections begin in 2021, it’s important to note that the effects of the COVID-19 pandemic on the workforce might not be fully reflected.
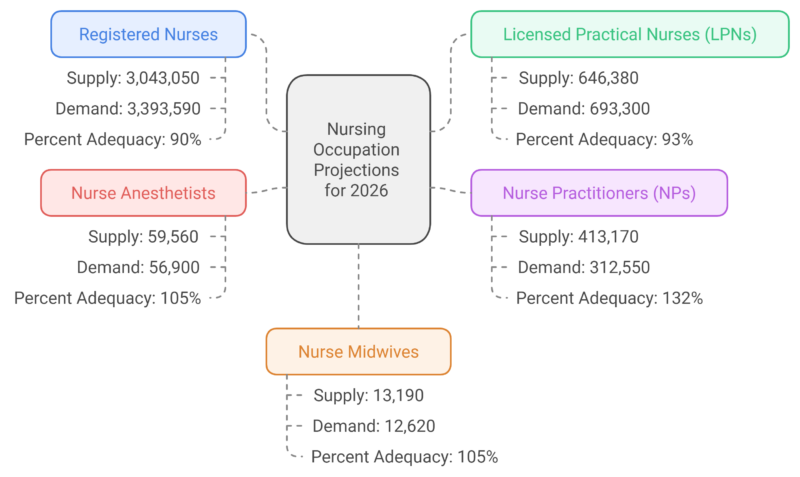
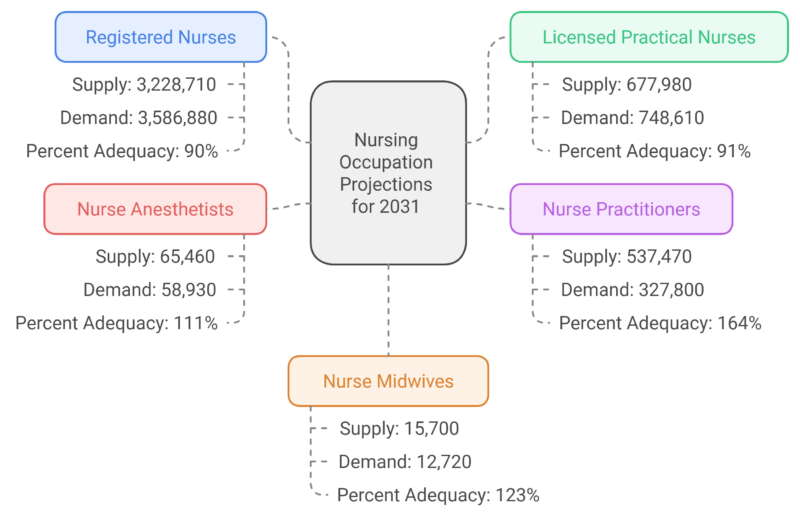
- National Shortage of Registered Nurses (RNs): A projected shortage of RNs will persist through 2036. There is an estimated 10% shortage in 2026 and 2031, improving slightly to a 9% shortage by 2036. By then, there will be a deficit of 337,970 full-time equivalent (FTE) RNs.
- Urban vs. Rural Divide: Rural and non-metropolitan areas are expected to experience a larger nursing shortage compared to metro areas. In 2026, rural areas face a 22% shortage, compared to an 8% shortage in metro regions. By 2036, the rural shortfall will be 14%, while metro areas will see an 8% deficit.
- Shortage of Licensed Practical/Vocational Nurses (LPNs): The demand for LPNs is projected to grow faster than the supply, leading to a shortfall of 99,070 LPN FTEs by 2036. Nationwide, by that year, the supply of LPNs will meet only 88% of the demand, down from 93% in 2026.
- Nurse Practitioners (NPs): On a positive note, the supply of NPs is expected to exceed demand throughout the projection period. However, geographic distribution remains a challenge, with some areas oversupplied while others face shortages.
By 2036, states like Georgia, California, and Washington are expected to have the largest deficits in RN supply, while some states will experience a surplus.
5 States with the Largest Projected Nursing Shortages
State
Projected RN Shortage (%)
Projected RN Shortage (FTEs)
Georgia
29%
-34,800
California
26%
-106,310
Washington
26%
-22,700
New Jersey
25%
-24,450
North Carolina
23%
-31,350
5 States with the Highest Projected Demand for Nurses
These states will have the highest absolute demand for nurses, although their shortages may not be the most severe in percentage terms:
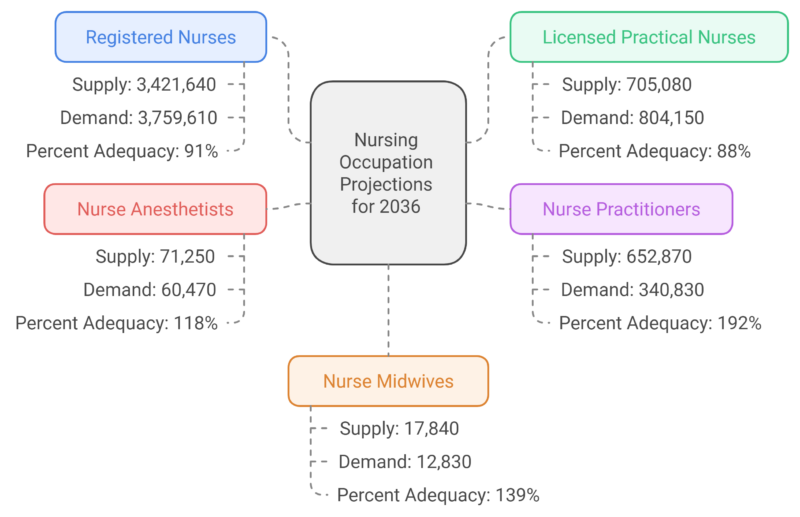
National Supply and Demand Projections for Key Nursing Roles
The following tables provide the projected supply and demand for selected nursing roles in 2026, 2031, and 2036:
Projections for 2026
Projections for 2031
Projections for 2036
Lowest Nursing Demand
On the other end of the spectrum, some states are projected to have the smallest nursing shortages by 2036.
Vermont is expected to have a deficit of just 230 registered nurses (RNs), followed closely by West Virginia, which will be short by 250 nurses, and Mississippi, falling 320 RNs short of meeting its demand.
Maine also has a relatively small shortage, with an estimated deficit of 390 nurses.
When ranked by the percentage of adequacy for nursing staff, Pennsylvania leads with over 99% adequacy, followed by Alaska (97%), Florida (just under 97%), Montana (slightly below 97%), and Illinois (just under 95%).
Additionally, several states are expected to experience no nursing shortage by 2036. North Dakota, for example, is projected to have 3,550 more nurses than needed, amounting to a 42% surplus.
South Dakota is forecasted to have 4,020 extra RNs, which equals a nearly 40% surplus. Utah will have a surplus of 6,180 nurses, equivalent to 17%, while Minnesota will have 10,520 more nurses than required, translating to a 16.5% surplus.
In general, the Northeast will have the lowest rate of nursing shortages, with a deficit rate of 6.6%, though the region still faces a net shortage of 36,510 nurses.
In contrast, the Midwest is the only region expected to have a surplus of nurses, with a 7.36% surplus, or 7,050 extra nurses.
Projections of Shortage By State
State
Supply of Registered Nurses
Demand for Registered Nurses
Nursing Shortage Percentage
Net Nursing Staff Shortages
Alabama
64,250
59,760
-8%
4,490 surplus
Alaska
7,960
7,760
-3%
200 surplus
Arizona
76,110
83,840
9%
-7,730
Arkansas
33,480
37,010
10%
-3,530
California
294,890
401,200
26%
-106,310
Colorado
60,040
63,520
5%
-3,480
Connecticut
36,440
42,720
15%
-6,280
Delaware
11,920
12,520
5%
-600
District of Columbia
7,230
6,430
-12%
800 surplus
Florida
290,230
281,680
-3%
8,550 surplus
Georgia
86,010
120,810
29%
-34,800
Hawaii
12,260
14,000
12%
-1,740
Idaho
19,210
22,860
16%
-3,650
Illinois
130,920
124,560
-5%
6,360 surplus
Indiana
73,450
79,000
7%
-5,550
Iowa
38,210
36,190
-6%
2,020 surplus
Kansas
35,980
36,750
2%
-770
Kentucky
52,170
55,980
7%
-3,810
Louisiana
47,590
55,250
14%
-7,660
Maine
17,750
18,140
2%
-390
Maryland
58,190
72,890
20%
-14,700
Massachusetts
75,140
80,430
7%
-5,290
Michigan
93,270
115,140
19%
-21,870
Minnesota
74,230
63,710
-17%
10,520 surplus
Mississippi
35,300
35,620
1%
-320
Missouri
70,850
71,950
2%
-1,100
Montana
13,060
12,650
-3%
410 surplus
Nebraska
23,600
21,720
-9%
1,880 surplus
Nevada
30,120
31,590
5%
-1,470
New Hampshire
14,030
18,150
23%
-4,120
New Jersey
74,400
98,850
25%
-24,450
New Mexico
19,430
22,500
14%
-3,070
New York
210,630
222,140
5%
-11,510
North Carolina
103,060
134,410
23%
-31,350
North Dakota
11,990
8,440
-42%
3,550 surplus
Ohio
151,390
138,650
-9%
12,740 surplus
Oklahoma
39,100
46,040
15%
-6,940
Oregon
38,040
45,450
16%
-7,410
Pennsylvania
149,910
148,480
-1%
1,430 surplus
Rhode Island
13,340
12,040
-11%
1,300 surplus
South Carolina
50,260
63,830
21%
-13,570
South Dakota
14,440
10,420
-39%
4,020 surplus
Tennessee
80,170
85,870
7%
-5,700
Texas
288,820
320,920
10%
-32,100
Utah
42,480
36,300
-17%
6,180 surplus
Vermont
6,950
7,180
3%
-230
Virginia
91,810
94,900
3%
-3,090
Washington
65,160
87,860
26%
-22,700
West Virginia
21,870
22,120
1%
-250
Wisconsin
58,280
63,180
8%
-4,900
Wyoming
6,220
6,200
0%
20 surplus
Why Is There a Nursing Shortage in the US?
While it’s a promising time for aspiring nurses and professionals aiming for leadership roles in education, administration, and management, the U.S. is still grappling with a significant nursing shortage, particularly as experienced nurses retire in large numbers.
This makes it an ideal moment for those considering higher education in nursing or healthcare leadership roles, such as those offered through Lamar University Healthcare programs, to address these pressing needs.
With an aging population that requires more complex and specialized care, nursing teams must grow in size and skill. Nurses need to be better prepared for challenging environments, manage more difficult patient needs, and adapt to higher standards and new healthcare technologies.

Several key factors contribute to the ongoing nursing shortage:
- Aging Population: As the population ages, demand for complex care is rising, particularly for chronic conditions. The number of Americans aged 65 and older is projected to grow faster than any other age group between 2024 and 2054 according to CBO. By 2054, this group will have doubled in size compared to 1973, reaching 74 million people.
- Retirement of Experienced Nurses: More than 1 million nurses are expected to retire by 2030. Over 50% of RNs are currently aged 50 or older, with the average age being 52, according to the National Nursing Workforce Study.
- Slow Growth in Nursing School Enrollment: Nursing school enrollment isn’t expanding quickly enough to meet the growing demand for RNs and Advanced Practice Registered Nurses (APRNs). The healthcare industry also faces a shortage of nurse educators, researchers, and primary care providers.
- Impact of Gender Dynamics: Since the majority of nurses are women (over 86%, according to the National League for Nursing), many leave or reduce their hours during childbearing years. While some return, others transition into different careers.
- Workplace Violence and Bullying: Ongoing bullying and violence in healthcare settings can deter new and current nurses from staying in or pursuing nursing careers, as highlighted in a study by the National Library of Medicine.
- Shortage of Nursing Faculty: The lack of nursing faculty limits the number of future nurses who can be trained. The American Association of Colleges of Nursing reports that nearly 92,000 qualified applicants were turned away from nursing programs in 2021-2022 due to faculty shortages, as well as a lack of clinical sites, classroom space, and funding.
- Nurse Burnout and Stress: Insufficient staffing leads to burnout, decreased job satisfaction, and higher turnover among RNs. Studies show that better nurse-to-patient ratios, enhanced nursing education, and empowering nurses are linked to improved patient outcomes, fewer medical errors, lower mortality rates, and reduced nursing shortages.
References:
- Bureau of Labor Statistics (BLS) – Healthcare Occupations in 2022
- Bureau of Labor Statistics (BLS) – Fastest-Growing Occupations
- Health Workforce Simulation Model (HWSM) – Nursing Projections Factsheet
- CBO – Population Projections
- Health Affairs – Retiring Baby Boomer Nurses
- National League for Nursing – Annual Survey 2021-2022
- National Library of Medicine – Workplace Violence and Bullying in Healthcare
- American Association of Colleges of Nursing (AACN) – Nursing Shortage Fact Sheet
Related Posts:
- Top 10 Healthcare Careers in Demand for 2025 -…
- What Percentage of Americans Are Registered to Vote in 2025?
- Utah Ranks in Top 5 Growth States as US Population…
- US States With the Highest Homeowners Insurance…
- 10 US. States With the Highest Alcoholism Rates in 2025
- 10 Highest-IQ States in the US for 2025 - What the…